
 http://orcid.org/0000-0001-8592-8980
http://orcid.org/0000-0001-8592-8980
Abstract. As young people are a vulnerable group, the prevalence of mental disorders in the population has been rapidly increasing in recent years. Not only are young people more at risk from mental disorders, but their lifelong burden accumulates for an extended period. Currently, the scale of the problem is enormous. Thus, various organisations and interest groups sound the alarm about the ongoing mental health crisis.[1]
This study aims to investigate the scale of youth mental health crisis in the context of socioeconomic development. The focus is on the burden on society, the economy, and progress as the underlying problems. The assessment is performed by literature studies and exploratory data analysis that allow for highlighting the ongoing tendencies and new phenomena concerning risk factors and mental disorders of young people, both globally and focusing on the Polish perspective, as well as evaluating the availability of mental healthcare in Poland, Europe, and the world.
The results indicate that mental health and well-being have not been considered healthcare priorities for a long time. In particular, three issues deserve special attention in the youth mental health crisis context. Firstly, addictions, especially Internet- and smartphone-related behavioural dependences, are becoming a global pandemic among young people. Secondly, the impact of the COVID-19 pandemic proved to be catastrophic for the mental health of children and adolescents. Finally, the available mental healthcare and its quality are inadequate to meet the growing needs of young people in the modern world.
Keywords: youth mental health, mental disorders, addiction, social burden of mental disorders, health economics, youth mental health in Poland, mental healthcare, socioeconomic development, regional studies
As the World Health Organization (WHO) highlighted, mental health is vital in personal and public health and well-being, a fundamental human right, and a crucial sustainable development priority (World Mental Health Report 2022). Mental, psychological, or psychiatric issues are detrimental to maintaining a high level of health, well-being, and quality of life. The WHO specifies numerous mental, behavioural, or neurodevelopmental disorders (referred to in this paper as mental disorders, diseases, illnesses or conditions, for short) broadly defined as clinically significant disturbances of a person’s cognition, emotional regulation, or behaviour. (ICD-11 2023; WHO 2022a) Estimates indicate that one in eight people (i.e. almost 1 billion people worldwide) has a mental disorder, with depression and anxiety being the leading conditions. Another statistic shows that one in 100 deaths is attributed to suicide, and there may be as many as 20 attempts per every successful one (Depression and Other 2017; GBD 2019; Mental 2022; World Mental Health Report 2022).
The burden, both social and economic, due to mental disorders is enormous. Mental illnesses are the leading cause of years lived with disability (YLDs) (around 15% of total YLDs) and premature deaths. These conditions lead to over US$1 trillion annually in economic losses, as mental health and well-being are crucial components of human capital. Most mental and behavioural diseases are chronic, and treatment and therapy are considered expensive (both “per person” and aggregated population-wise). However, as proven by comparative studies, the lost productivity and socioeconomic burden of mental health conditions greatly outweigh total healthcare expenditures, and yet most countries tend to prioritise other health issues (i.e. cardiovascular diseases, neoplasms) (Iordache et al. 2023; World Mental Health Report 2022).
While mental disorders and their underlying risk factors can occur throughout the life cycle, youth is the most sensitive period due to ongoing physical, psychosocial and cognitive development. For instance, children and adolescents’ long-term exposure to stressful situations, such as family conflict, bullying at school, or cyberbullying via social media, is likely to cause damaging effects on developing core cognitive and emotional skills, leading to various mental and behavioural illnesses. Youth[1] subjected to stress tend to die prematurely within 20 years compared to the general population. As young people are a vulnerable group, the prevalence of mental disorders in the population has been rapidly increasing in recent years. Not only are the young people more at risk from mental disorders, but their lifelong burden (individual and aggregated over the whole population) is also much higher than for the older cohorts as YLDs, lost productivity, and healthcare expenditures accumulate for an extended period. Currently, the scale of the problem is enormous. Thus, various organisations and interest groups sound the alarm about the ongoing mental health crisis (WHO: Factsheet for World Mental Health Day 2018; Wolf et al. 2018).
Hence, this study aims to investigate the scale of youth’s mental health crisis in the context of socioeconomic development.[2] The focus is on the burden on society, the economy, and progress as the underlying problems. The assessment is performed by literature studies and exploratory data analysis that allow for highlighting the ongoing tendencies and new phenomena concerning risk factors and mental disorders of young people, first globally (Section 2) and, subsequently, focusing on the Polish perspective (Section 3), as well as evaluating the availability of mental healthcare in Poland, Europe, and the world (Section 4). The final section of the paper offers a summary and conclusions.
Assessing global tendencies of the mental health crisis of young people allows us to identify the focal points, such as increasing prevalence, self-harm and suicide, addictions, stress-related issues, as well as the impact of the COVID-19 pandemic and restrictions on mental youth well-being.
Estimates indicate that more than 0.25 billion, that is, one in seven children and adolescents, are hindered by some mental condition.[3] Mental disorders account for around 13% of the global disease burden among youth, and around half of mental health conditions develop by age 14. Poor mental health is the leading cause of disability for youth. Unfortunately, a significant share of these conditions is undiagnosed and untreated. Additionally, numerous young people suffer from psychosocial issues that do not fulfil a clinical disorder’s diagnostic criteria, diminishing their quality of life and mental well-being and hindering future life. (UNICEF[4] 2023; WHO 2020; 2021b).
Global Burden of Disease Study 2019 (GBD 2019) indicates that the socioeconomic burden due to mental disorders for young people is high and increases over time. In the case of young men and women, the disability-adjusted life years (DALYs) per 100,000 people in 2019 were elevated in developed regions of the Americas, Europe, Mediterranean and Australia. In particular, for females, the mental disorder burden was the highest in the Iberian Peninsula and Western Europe, while for males in Australia, New Zealand, Portugal, Greece and some Middle Eastern states. (Fig. 1a and 2a) The share of the mental disorders DALYs in the total DALYs is the highest in Western and Northern Europe, Australia, and Japan. (Fig. 1b and 2b) In almost all countries, the burden of mental disorders among young people increases systematically over time, with the greatest increments in the Americas (especially the United States) and Africa (Fig. 1c and 2c). Notably, the DALYs burden of mental illnesses grows with the level of regional development; hence, it is the largest for both genders under 20 years in high-income countries. The social cost of anxiety and depression seems to increase for the richest states (Fig. 3).
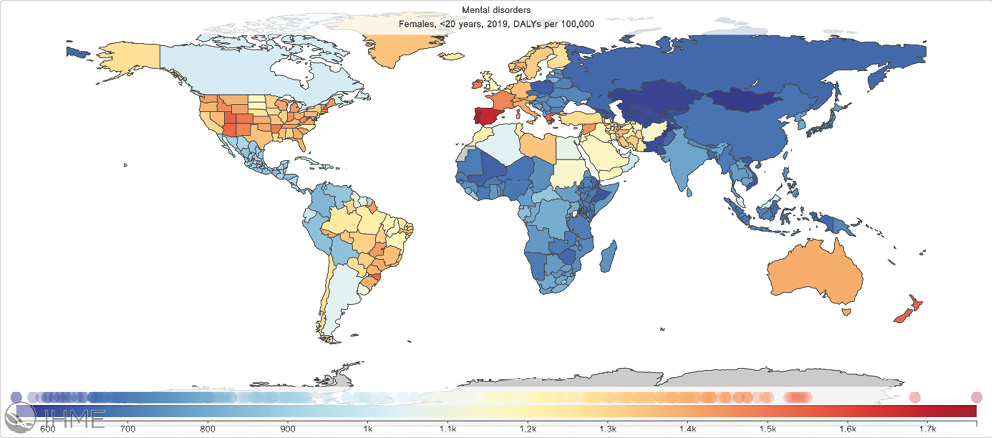
a. number of mental disorders DALYs
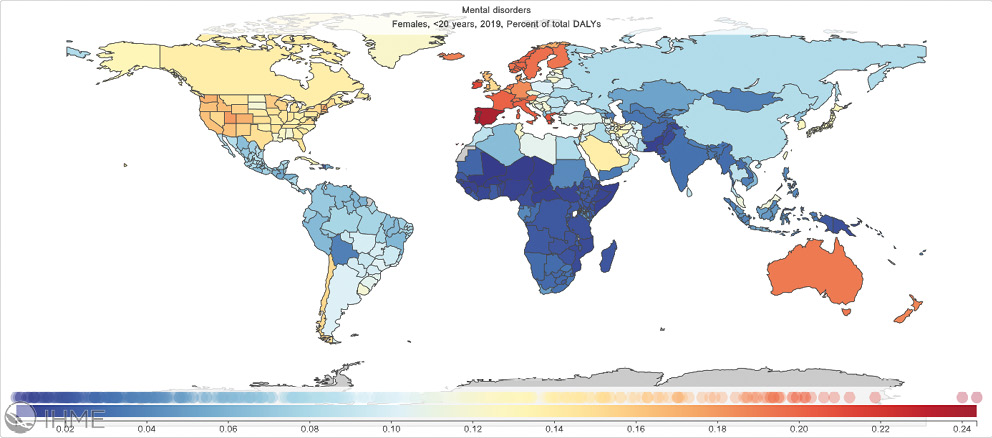
b. share of mental disorders DALYs in the total DALYs
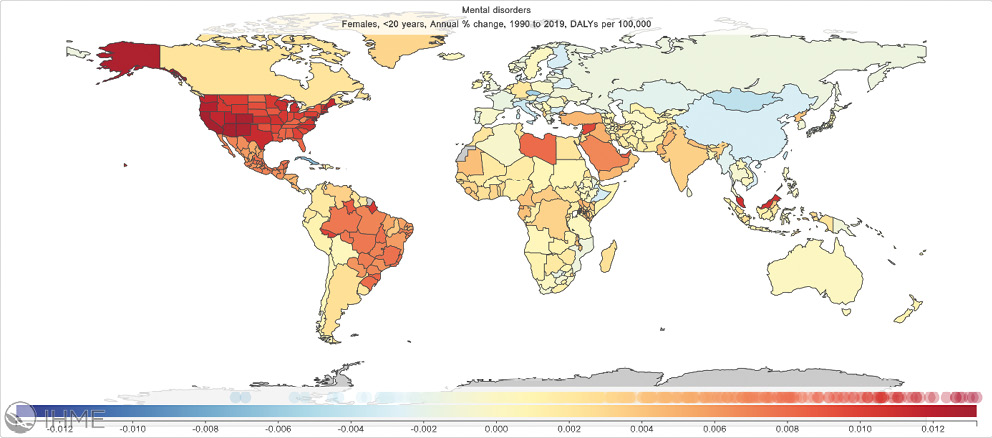
c. annual percentage change of mental disorder DALYs 1990–2019
Fig. 1. Female under 20 years of age mental disorders burden measured by disability-adjusted life years (DALYs) per 100,000 people, 2019
Source: GDB 2019.
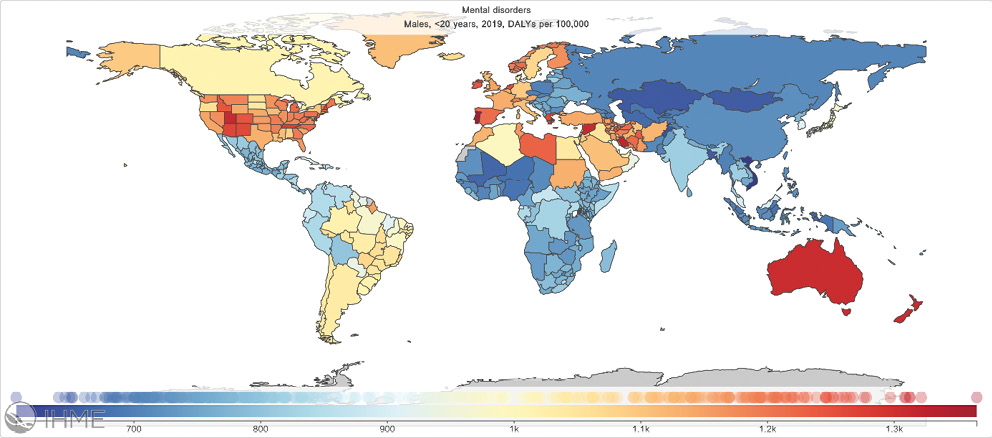
a. number of mental disorders DALYs
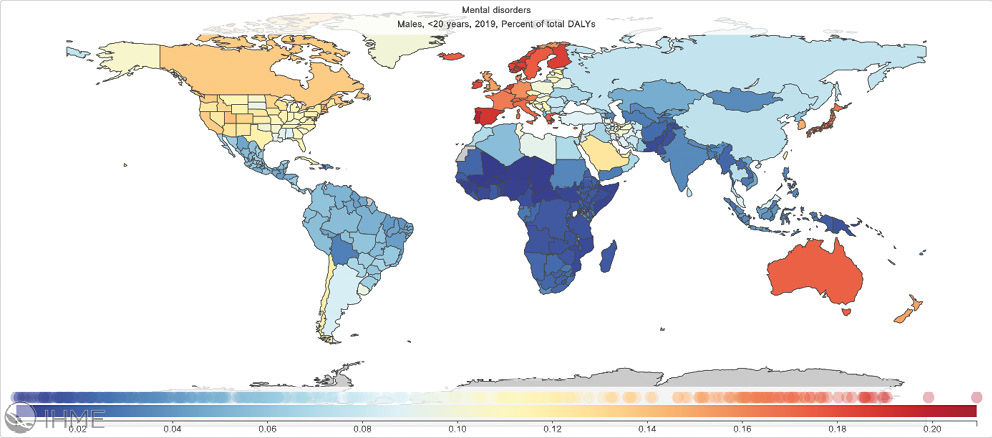
b. share of mental disorders DALYs in the total DALYs
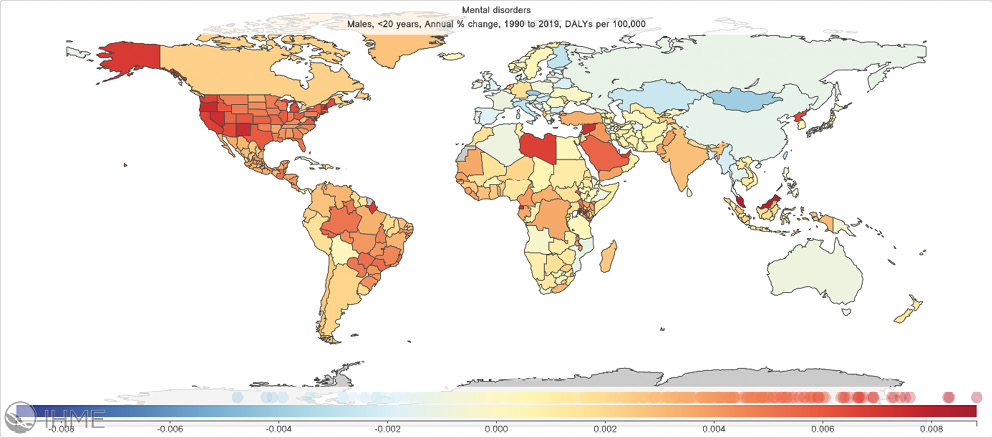
c. annual percentage change of mental disorder DALYs 1990–2019
Fig. 2. Male under 20 years of age mental disorders burden measured by disability-adjusted life years (DALYs) per 100,000 people, 2019
Source: GDB 2019.
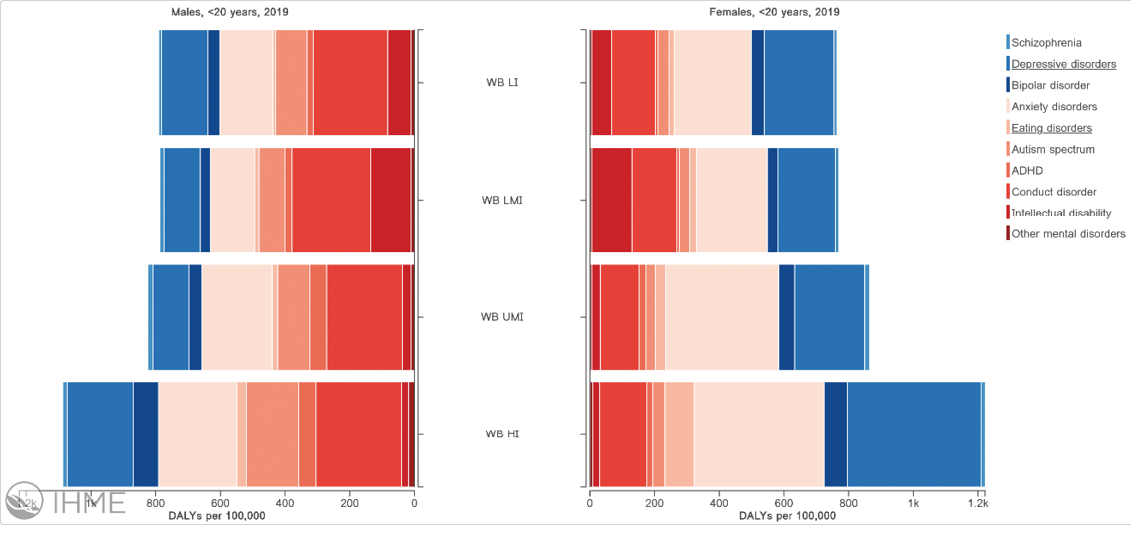
Fig. 3. Male and female under 20 years of age mental disorders burden measured by disability-adjusted life years (DALYs) per 100,000 people, by World Bank country income groups, 2019 (Worlds Bank (WB): LI – low-income countries, LMI – low-middle income, UMI – upper-middle income, HI – high-income countries group)
Source: GDB 2019.
Suicide is another critical mental issue addressed in the United Nations Sustainable Development Goals (SDGs) and WHO’s Comprehensive Mental Health Action Plan 2013–2030. While 77% of suicides occurred in low- and middle-income countries where most of the world population lives, the highest age-standardised suicide rate of 10.9 per 100,000 is observed in high-income countries. For youth, suicide constitutes the third (female) or fourth (male) leading cause of death (Training manual 2022).
Addictions are also conditions for which the youth are the highest risk group. Numerous studies indicate that behavioural dependences may have become the modern epidemic among young people. Sharma et al. study (2023) suggest the prevalence of smartphone dependence among adolescents at 23% with 77.2% comorbidity with depression. Regarding Internet use, various studies show dependency frequency between 4.9% and 56.9% of youth (Bekar, Arıkan, Çapık 2022). A survey by Allahverdi (2022) indicates that 70% of students self-report being addicted to social media, with a significantly higher share of females. The prevalence of online gaming addiction varies from 0.6% to over 22% in the young population (Hu 2022).
Natural disasters, military conflicts and other emergencies have a detrimental impact on mental health, and the consequences more severely burden vulnerable groups like children and adolescents. (Gawrych 2022; Goto et al. 2023) The mental health and well-being of most people in the world have been temporarily or permanently impacted by the COVID-19 (or SARS-Cov-2) pandemic and subsequent restrictions (social distancing, lockdowns, online schooling, studying and working, limited access to mental healthcare) that occurred worldwide between 2019 and 2022. WHO estimates indicate that globally, in 2020 alone, the COVID-19 pandemic has led to a prevalence increase of 27.6% for depressive disorder (with 137.1 additional disability-adjusted life years – DALYs per 100,000 population) and 25.6% for anxiety disorders (with added 116.1 DALYs per 100,000 population). Moreover, individuals with preexisting mental disorders were at greater risk of severe illness and death from COVID-19 and should have been considered a risk group upon diagnosis of infection. As data indicate, females and youth, especially those aged 20–24, were more affected than males and older adults (Mental Health and COVID-19 2022).
Children and adolescents have suffered dramatically during the COVID-19 pandemic from the sudden withdrawal from school, social life, and outdoor activities. Some of them have also experienced increasing domestic violence. Young people’s stress during the period directly affected their mental health due to increased anxiety and fear (Chałupnik et al. 2022). Besides the adverse effects of COVID-19 and its burden, children, adolescents and young adults were psychologically affected by lockdowns with boredom, loneliness, frustration, irritability, quarrelsomeness, restlessness, sadness, anger, and worry, which were detrimental to their mental well-being. Even post-traumatic stress symptoms were diagnosed as a result (Abdulah, Piro 2022; Brooks et al. 2020; Carey, Povey, Taylor 2022; Layachi, Schuelka 2022; Morgül, Kallitsoglou, Essau 2020). It has also been noticed that children and adolescents were less likely to report worsening mental health than adults (Leigh et al. 2023). From the parents’ perspective, more than two-thirds declared that due to social isolation and lack of contact with peers, they witnessed a deterioration in their children’s emotional well-being (72%), behaviour (68%) and physical health (68%) (RPD 2023).
Numerous research highlighted increased Internet and smartphone use during the COVID-19 pandemic. As a result, the prevalence of internet addiction among adolescents increased significantly, as well as an addiction to online gaming for males and to social media for females (Carkaxhiu Bulut, Gokce 2023; Rathi, Guha, Neogi 2022; Yılmaz, Aydoğdu, Koçtürk 2022).
As COVID-19 is now not considered a worldwide public health emergency and most restrictions have ended, acute mental disorders are expected to decrease. However, many harmful psychological effects are likely long-term and will impact young people’s development and future choices.
An evident duality is present in Polish studies of youth’s psychological well-being. Before the COVID-19 pandemic, mental health epidemiological research was sparse and superficial, often based only on mortality and treatment statistics. The COVID-19 pandemic turned out to be a breakthrough in the perception of youth’s mental health in Poland. Both public and private institutions have carried out numerous survey studies.
In Poland, the deep interest in mental health in general, and of youth in particular, is a relatively new phenomenon. Tabak (2014) pointed out that over a decade ago, literature needed more methodological aspects and empirical results assessing the mental well-being of children and adolescents. Scarce existing mental health reports focused on adults or above 15 years, while public health research of the underaged only briefly mentioned psychological aspects. The research gap was a direct result of undervaluing mental conditions as well as related epidemiological studies for young people.
Available rudimentary data indicate that between 2005 and 2008, there was an upward trend in the incidence of mental disorders among children and adolescents, as measured by the number of people treated per 100,000 population. In 2008, patients aged 0–18 accounted for 9.2% of all patients treated in outpatient psychiatric care. The most common conditions among children and adolescents attending a mental health clinic were behavioural and emotional disorders (587,6 per 100,000 of the population) as well as stress-related neurotic disorders. The second leading cause of hospitalisation was disorders triggered by using psychoactive substances, the most common of which was addiction. An increased prevalence of illnesses caused by alcohol use in the youngest age group was noticed. Moreover, suicides were one of the dominant causes of death among youth and accounted for 12.2% of all suicides in Poland. In the 15–19 age group, a suicide attempt was the cause of death for 26% of males and 16% of females (Tabak 2014).
Research based on the Ministry of Health data showed that in 2011, 108,707 people aged 0–18 were treated for mental disorders other than addictions, constituting 1.3% of the age group. Nevertheless, parallel survey studies indicated that the prevalence of mental conditions exited 30%, with depression and eating disorders as leading issues. Significant discrepancies between the number of youth registered in treatment and the epidemiological research indicate that a substantial part of this population remained outside professional care (Tabak 2014).
Between 2014 and 2016, according to various sources, the share of children and adolescents with mental disorders needing professional care ranged from 9% to 15%. In 2014, the number of suicides of youth under 19 in Poland was in second place in Europe (Rudnik, Wachowiak 2020). In 2016, 42% of youth (48% for girls and 36% boys) exhibited symptoms of mental health disorders. Between 2008 and 2016, the percentage of young people experiencing internalising problems increased significantly. The leading cause was the increase in the prevalence of depressive symptoms (Bobrowski, Ostaszewski, Pisarska 2021).
The COVID-19 pandemic has undoubtedly changed the world as we know it in many ways. The disease’s cumulative socioeconomic costs are enormous, with excess deaths and the burden due to acute and long-term physical and psychological symptoms. However, as the prevalence of mental disorders, especially among young people, increased, so did the awareness and interest of medical professionals, society, socioeconomic researchers, non-governmental organisations (NGOs), and public institutions in Poland. As a result, numerous studies were performed over the years 2020–2023 concerning the wide range of mental well-being of children and adolescents, constituting an unexpected benefit of the COVID-19 pandemic.
Polish Ombudsmen for Children (pl. Rzecznik Praw Dziecka, RPD), among other activities, studies the health of children and adolescents in Poland. The RPD 2021 and RPD 2023 reports focus on mental well-being. 80% of school children assess their mental functioning as good without needing external intervention. Among those experiencing some mental issues, the most prevalent problems are often not wanting to do anything (32%) or feeling sad (29%). It has been noted that mental health self-assessment among Polish students deteriorates with age, and girls are particularly vulnerable to declining self-esteem. A supplementary study on parents indicated that they overlook the full extent of children’s mental problems or the decline of well-being over time. For instance, while 37% of youth feel lonely, only 17% of parents observe this problem in their children. In the context of the COVID-19 pandemic and related restrictions, data analysis from the Children’s Helpline of the Ombudsman showed an increase in the frequency of anxiety, tension, and loneliness.
Alternative, independent research is mainly carried out by NGOs, research institutions, and some with media cooperation. These studies are often comprehensive in assessing the youth’s mental well-being. Among them are the reports by Empowering Children Foundation (pl. Fundacja Dajemy Dzieciom Siłę), UNAWEZA Foundation, Health Education and Psychotherapy Foundation (pl. Fundacja Edukacji Zdrowotnej i Psychoterapii), and Difference ordered by Radio Zet deserve special attention.
Empowering Children Foundation reports indicate that the number of children and adolescents covered by specialist assistance due to mental disorders has been growing in recent years. A study in 2021 of children and adolescents aged 7–17 estimated that internalising disorders (e.g. fears, phobias) may affect 7.3% of people, affective disorders (e.g. depression, mania) – 1.7%, and externalising disorders (e.g. behaviour, oppositional defiant behaviour, ADHD) – 4%. Eating disorders affected 2.6% of this group, and conditions related to the use of psychoactive substances – 4.2%. Suicide thoughts were experienced by 5.7%. Overall, internalising disorders prevailed among younger children, while among adolescents – externalising disorders peaked around 16–17 years of age. LGBT+ youth are a vulnerable group in Poland – 75% of non-heteronormative teenagers feel lonely, 41% often have suicidal thoughts, and 55% exhibit at least moderate symptoms of depression, only 22% have a sense of acceptance on the part of their mothers and 12% – on the part of their fathers (Makaruk, Włodarczyk, Szredzińska 2020; Szredzińska 2022).
According to the Empowering Children Foundation studies during the first wave of the pandemic, 30% of youth aged 11–17 negatively assessed their satisfaction with life during this period, with the leading causes of the mental well-being decline being lack of contact with peers, the need to sit at home, and remote learning. Suicide, suicide attempts, and self-harm are notable benchmarks of the mental health crisis. Generally, those statistics are high in Poland. In 2021, suicide was the second leading cause of death among teenagers aged 15–19 (i.e. 20% of all deaths in this age group). During the first lockdown between March and June 2020, nearly 3% of respondents aged 15–17 tried to take their own lives, and 9.2% of youth admitted that they had experienced intentional self-mutilation (Makaruk et al. 2020; Szredzińska 2022).
UNAWEZA Foundation Report (Dęsbki, Flis 2023) indicates that the most common mental issues of Polish youth are: lack of motivation to act (declared by 52.4% of respondents), feelings of loneliness (37.5%), problems sleeping (37%), lack of self-acceptance (32.5%), learning problems (31%), and no will to live (28%). Among risky behaviours, the most prevalent seems to be trying to lose weight regularly (32.8%) and self-harm (16%). Almost half (46%) of young people have extremely low self-esteem, and 27.4% believe their value depends on the acceptance of others, while 10.5% feel that no single person fully accepts them. External threats include online hate experienced by almost half of children and adolescents, peer violence that 9.5% of respondents deal with, feeling neglected by their parents (11.5%), and being victim to domestic violence (acknowledged by 4.5%).
A Health Education and Psychotherapy Foundation report shows that 43% of adolescents declare difficulties related to mental health. In particular, 75% of respondents worry about the future, 62% have trouble sleeping, 43% think about death, and 70% feel more nervous and irritable than before the COVID-19 pandemic, restrictions, and online schooling (Białecka 2021). These alarming statistics are confirmed in the Difference (2021) report ordered by Radio Zet. Furthermore, the COVID-19 pandemic resulted in online schooling and transferring social activities and entertainment online and, as Sikorska et al. (2021) study proved, increased time spent in a virtual environment corresponds with higher levels of depression, anxiety, and stress. The duration of online activity is also negatively correlated with psychological, emotional, and social well-being.
Essential factors in assessing mental health and well-being are the availability and accessibility of mental healthcare, its resources and financing, the quality of professional aid, and the level of meeting mental health needs.
Globally, the median number of mental health workforces is 13 per 100,000 population in 2019, with high dispersion over World Bank states’ income groups. Recorded values vary between below two in low-income and 60 per 100,000 population in high-income countries (Mental health atlas 2020). In Europe, in 2021, the median number of psychiatrists per 100,000 population was almost 17, ranging from 6.63 in Turkey to 52.88 in Switzerland (Fig. 4). In the long term, the number of psychiatrists increased in most European countries. In Poland, there were only 13.02 psychiatrists per 100,000 people (Eurostat data). The most current data (30.04.2023) of the Supreme Medical Chamber (pl. Naczelna Izba Lekarska) indicate that in Poland, there are 4554 practising psychiatrists, that is 14.95 per 100,000 of the adult population and 543 active children and adolescent’s psychiatrist – thus there are 9.57 doctors per 100,000 underaged inhabitants or 10,444.58 potential patients per one doctor. These statistics indicate that the availability of youth mental care in Poland is dramatically low (Naczelna Izba Lekarska; Baza Demografia).
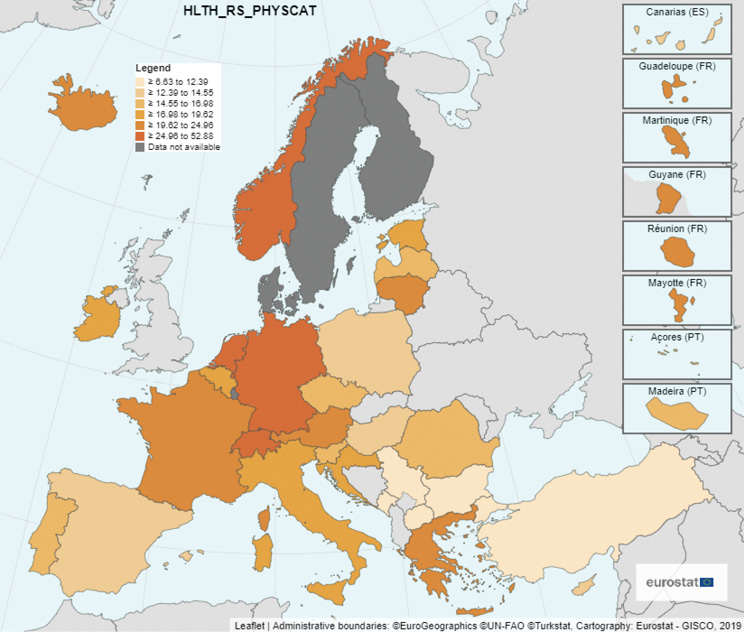
Fig. 4. Number of psychiatrists per 100,000 inhabitants, 2021
Source: Eurostat data.
According to WHO, the median number of mental hospital beds per 100,000 population varies between income groups, from around two in low-income countries to over 25 in high-income countries. Globally, the median number of mental hospital beds reported per 100,000 population increased from 6.5 beds in 2014 to 11 beds in 2020 (Mental health atlas 2020). In Europe, in 2021, the median was 74.65 beds, after a 12% decline compared to 2003. In Poland, the number of beds declined by 15% between 2003 and 2021, placing it in the European bottom quartile with 60.68 beds per 100,000 inhabitants (Fig. 5, Eurostat data).
In the case of youth mental healthcare in Poland, in 2019, in five provinces (i.e. Lubuskie, Opolskie, Świętokrzyskie, Warmińsko-Mazurskie and Zachodniopomorskie), there was not a single psychiatric day care ward for children and adolescents, and in Podlaskie there was no inpatient ward. Depending on the province, there were 2,155 to 13,537 children per bed in inpatient care (Szredzińska 2022).
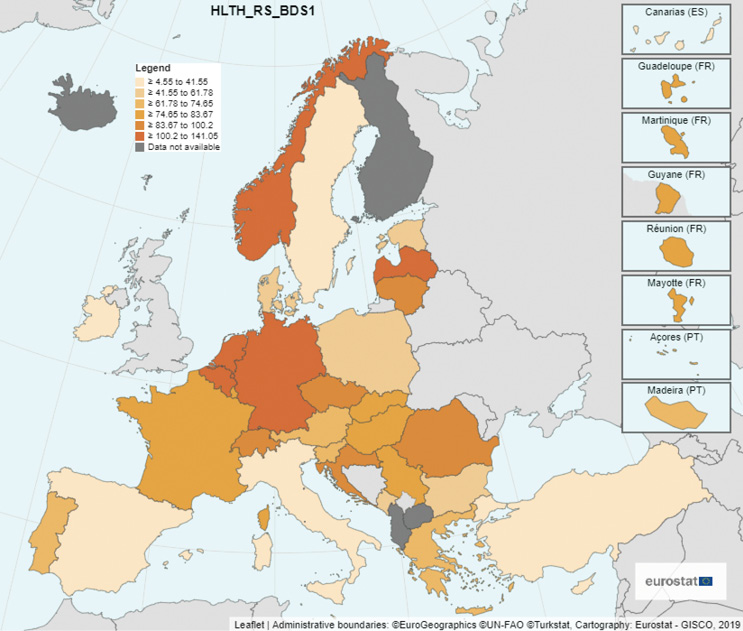
Fig. 5. Number of hospital beds in psychiatric care per 100,000 inhabitants, 2021
Source: Eurostat data.
Public expenditure on mental health is low worldwide, with a global median of 2.1% of government total health expenditure, especially in low- and middle-income countries (Mental health atlas 2020). Mental healthcare expenditures, for the most part, are directed at mental hospitals. In Europe, in the case of psychiatric hospitals, the spending per capita varied significantly in 2020 between 0.88 in Finland and 406.21 purchase power standard euro (PPS) in Norway. Polish expenses were below the median value at almost 19 PPS per person (Fig. 6). In most states, the expenditures tend to rise over time, but Poland experienced a slight decline from 2011 to 2021. Mental hospital expenses constitute 1.19% of the total Polish healthcare expenses, slightly below Europe’s median value (Eurostat data).
Unfortunately, statistical and financial data are not gathered or easily accessible for youth mental healthcare. Considering the ongoing mental health crisis of children and adolescents, special attention should be given to a relevant subdivision of resource information.
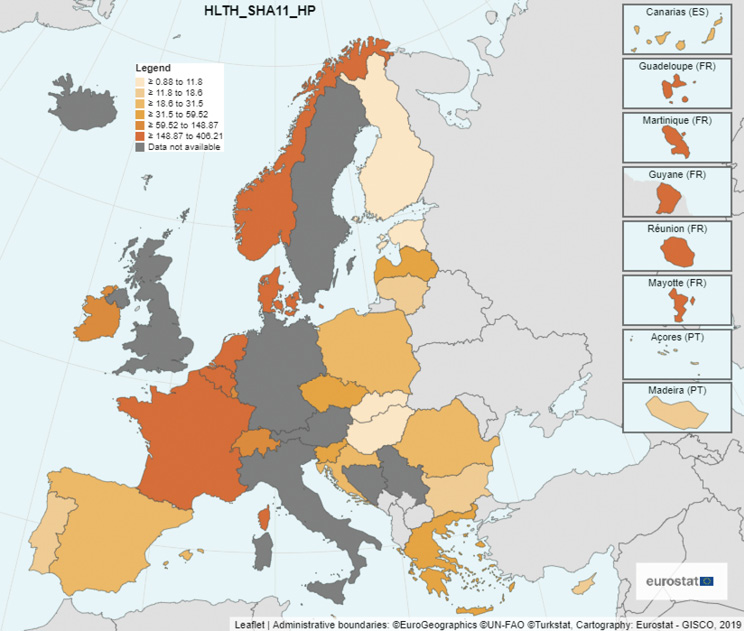
Fig. 6. Healthcare expenditure on mental hospitals, 2020 (purchasing power standard (PPS) per inhabitant)
Source: Eurostat data.
According to the WHO World Mental Health Report (2022), countries contribute less than 2% of their healthcare expenditures to mental health on average. In middle-income states, over 70% of mental health spending is directed at psychiatric hospitals, which have limited efficiency in treating a wide range of mental conditions, including mood disorders, addictions, and neurodevelopment illnesses. From a global perspective, more than half the world population lives in regions with less than 0.5 psychiatrists per 100,000 and limited availability of essential psychotropic medicines. In many countries, particularly low-income, there are no formal mental health services, and often, even if available, they are inaccessible or unaffordable. Due to persisting discrimination, ostracism, and stigmatisation, people frequently choose to suffer mental distress without relief rather than utilise mental health services. Even in states with reasonably high levels of mental healthcare, there are gaps in service coverage and variability in quality of care across regions and socioeconomic groups. As a result, a high share of people with mental conditions are not diagnosed, and most of the diagnosed go entirely untreated (World Mental Health Report 2022).
In Poland, as demonstrated by the Supreme Chamber of Control (pl. Najwyższa Izba Kontroli, NIK) investigation of psychiatric treatment availability for children and adolescents in 2017–2019, mental healthcare does not meet the needs. It does not provide comprehensive and universally accessible psychiatric support (NIK 2019).
The COVID-19 pandemic not only had a significant impact on the mental health and well-being of youth but also on the functioning of the healthcare system. The lockdowns and transfer of resources to epidemiological facilities severely disrupted mental health services, and the treatment gap for mental health conditions has widened (World Mental Health Report 2022). One-third of countries reported complete or partial disruption of delivery of mental, neurological and substance use interventions. 35% of states declared that even life-saving emergency and essential services were affected, while 30% indicated interruption in the supply of related medications. As a result, only around 30% of mental health services for children and adolescents were available with no disruption (The impact of COVID-19 2020).
In Poland in 2020, the inpatient psychiatric care for children and adolescents was mainly interventional. Only 22% of children’s admissions were planned in psychiatric wards, while 74% concerned emergency cases. This admittance structure means that the system shifted from treating diseases to crisis and life-threatening situations management. Waiting time for psychiatric help for youth was extensive – 66 to 330 days for stable cases and 8–213 days for emergencies (Szredzińska 2022).
As presented, the mental healthcare of youth is dramatically lacking in Poland, Europe, and the world. The financial resources, facilities and medical specialists are insufficient to battle the mental health crisis that haunts young people around the globe. It can be argued that professional help is expensive, but failing to meet youth’s mental health needs generates enormous costs. For instance, a global lifelong income loss due to unaddressed children and adolescents’ mental health needs caused by humanitarian emergencies amounts to US$203 billion. Overall, estimates prove that the economic benefits of investing in mental healthcare and psychosocial support outweigh the implementation expenditures (UNICEF 2023).
Mental health and well-being have not been considered healthcare priorities for a long time. Despite the unequivocal advancement in understanding mental issues and establishing guidelines, the global improvement accomplished in this field over the last two decades has been insufficient to prevent and counteract the mental health crisis we now experience (World Mental Health Report 2022). Neglecting and underestimating the complexity and severity of mental conditions lead to a rapid rise in prevalence and low availability, accessibility, and quality of treatment. This problem is especially worrisome for children, adolescents and young adults for two reasons. Firstly, due to the lower social and psychological development level, they are more vulnerable to the impact of various risk factors and, thus, more likely to develop mental illnesses than adults. Secondly, falling ill with a mental condition at an early stage in life results in a higher life-long burden of the disease for the person, their loved ones, society, and the economy. Cumulative economic costs of youth mental health issues include private and public expenditures and loss of income and productivity. Social effects incorporate comorbidity with other psychological and physical diseases, loss of healthy life years, diminished quality of life, premature death, family difficulties, and disrupted social interactions.
In the youth mental health crisis context, three issues deserve special attention. Firstly, undoubtedly, the prevalence of mental illnesses among young people has been and, most likely, will continue to increase rapidly, but the structure of most common disorders evolves over time. Remarkably, Internet- and smartphone-related addiction have risen in frequency as the omnipresence of the smartphone and online activity is perceived as natural for the digital generation, making it difficult to distinguish pathological symptoms from ‘normal’ behaviours (Jeong, Suh, Gweon 2020).
The second key aspect of youth mental health that needs addressing is the impact of the COVID-19 pandemic. A very rapid increase in new mental symptoms and declining access to dedicated healthcare for both new and preexisting conditions has the unprecedented potential to undermine the health and well-being of young people worldwide. Evidence from past emergencies suggests potentially elevated risks of anxiety and depression, trauma, self-harm, and even suicide among adolescents (WHO 2022b). Due to non-sustainable regional development, natural disasters and extreme weather conditions caused by climate change, global and local epidemics and military conflicts have become more frequent. Hence, the prevalence of mental health conditions and related socioeconomic burdens will rapidly increase in the upcoming decades.
Finally, the available mental healthcare and its quality are inadequate to meet the growing needs of children and adolescents in the modern world. Moreover, the policies and system structure seem to be outdated as they do not employ the most effective treatment methods and fail to respond to the evolving social aspects and technological advancement that constitute fundamental determinants of the current mental health of young people.
Surprisingly, in Poland, the detrimental impact of pandemics on youth mental well-being advanced social awareness and initiated numerous studies into youth psychological problems. Unfortunately, as it turned out, the situation of the mental condition of young people and related healthcare proved to be dire. Numerous pandemic and post-pandemic studies indicate a rising prevalence of anxiety, depression, self-harm, suicide symptoms, and addiction, while the treatment continues to be scarce, insufficient, and underfunded. Thus, as a result, it can be expected that youths’ mental health and well-being in Poland will continue to decline.
As presented in the paper, the global youth mental health crisis should not be treated lightly. International organisations like WHO, UNICEF, UN and local NGOs sound the alarm, as the inevitable and constant social, economic, and technological progress is detrimental to the youth’s mental health. Rapid changes in the modern lifestyle and traumatic events (global, local, and individual) tend to impact children and adolescents’ psychosocial development negatively. Furthermore, those young people plagued with mental conditions will grow into adults hampered by internal problems. These grownups will constitute a society burdened with an unprecedented prevalence of a wide variety of mental disorders and associated tremendous social and economic costs. As the byproduct of the modern world’s progress, the current youth mental health crisis may be just the harbinger of future catastrophe if appropriate action is not taken immediately. The necessary changes should be multidimensional and address the underlying determinants and the diagnostics and treatment of young people.
Abdulah D.M., Piro R.S. (2022), Understanding the impact of home confinement on mental health, sleep, and behavior of children during the COVID-19 pandemic: a qualitative study, “Health Prob Civil.”, vol. 16(4), pp. 286–301. https://doi.org/10.5114/hpc.2022.121517
Allahverdi F.Z. (2022), Relationship between perceived social media addiction and social media applications frequency usage among university students, “Psychology in the Schools”, vol. 59(6), pp. 1075–1087. https://doi.org/10.1002/pits.22662
Bassi G., Lis A., Marci T., Salcuni S. (2023), The Italian Version of Smartphone Addiction Inventory (SPAI-I) for Adolescents: Confirmatory Factor Analysis and Relation with Self-Control and Internalised-Externalised Symptoms, “International Journal Mental Health and Addiction”, no. 21, pp. 1992–2005. https://doi.org/10.1007/s11469-021-00705-w
Baza Demografia, Statistics Poland, https://demografia.stat.gov.pl/bazademografia/Tables.aspx (accessed: 23.08.2023).
Bekar P., Arıkan D., Çapık C. (2022), The relationship of internet addiction with social media use purposes and loneliness of adolescents, “Journal of Educationand Research Nursing”, vol. 19(3), pp. 342–349.
Białecka B. (2021), Etat w sieci 2.0. Zdrowie psychiczne polskich nastolatków w nauce zdalnej [Full time on the web 2.0. Mental health of Polish teenagers in distance learning], Raport Fundacji Edukacji Zdrowotnej i Psychoterapii [Report of the Foundation for Health Education and Psychotherapy].
Bobrowski K.J., Ostaszewski K., Pisarska A. (2021), Zdrowie psychiczne warszawskich gimnazjalistów. Badania mokotowskie 2004–2016 [Mental health of Warsaw middle school students. Mokotow Study 2004–2016], “Psychiatria Polska”, vol. 55(1), pp. 127–143. https://doi.org/10.12740/PP/OnlineFirst/112215
Brooks S.K., Webster R.K., Smith L.E., Woodland L., Simon W., Greenberg N., Rubin G.J. (2020), The psychological impact of quarantine and how to reduce it: rapid review of the evidence, “The Lancet”, vol. 395(10227), pp. 912–920. https://doi.org/10.1016/S0140-6736(20)30460-8
Büyük E.T., Savaş Z.O. (2022), Effect of Internet Addiction on the Sleep Quality of Adolescents During COVID-19 Pandemia Duration Period, “Journal of Turkish Sleep Medicine”, no. 9, pp. 232–237. https://doi.org/10.4274/jtsm.galenos.2022.42104
Carey A., Povey R., Taylor J. (2022), ‘Waiting out the day, not living, not fun’: a qualitative investigation of children’s experiences of school closures due to COVID-19, “Preventing School Failure: Alternative Education for Children and Youth”, vol. 67(3), pp. 181–194. https://doi.org/10.1080/1045988X.2022.2132199
Carkaxhiu Bulut G., Gokce S. (2023), Problematic social media use, digital gaming addiction and excessive screen time among Turkish adolescents during remote schooling: implications on mental and academic well-being, “Marmara Medical Journal”, vol. 36(1), pp. 24–33. https://doi.org/10.5472/marumj.1244628
Chałupnik A., Borkowska A., Chilimoniuk Z., Dobosz M., Wieteska M., Mizerski G. (2022), Impact of the COVID-19 pandemic on the mental health of selected population groups, “Journal of Education, Health and Sport”, vol. 12(3), pp. 32–41. https://doi.org/10.12775/JEHS.2022.12.03.003
Chi X., Hong X., Chen X. (2020), Profiles and sociodemographic correlates of internet addiction in early adolescents in Southern China, “Addict Behav”, no. 106, 106385.
Depression and Other Common Mental Disorders: Global Health Estimates, (2017), World Health Organization, Geneva.
Dębski M., Flis J. (2023), MŁODE GŁOWY. Otwarcie o zdrowiu psychicznym. Raport z badania dotyczącego zdrowia psychicznego, poczucia własnej wartości i sprawczości wśród młodych ludzi w Polsce [YOUNG HEADS. Opening up about mental health. Report from a study on mental health, self-esteem and agency among young people in Poland], UNAWEZA Foundation, Warsaw.
Difference (2021), Dzieci w pandemii. Raport z badania ilościowego na zlecenie Radia Zet [Children in a pandemic. Quantitative research report commissioned by Radio Zet]. https://newsroom.eurozet.pl/141891-dzieci-w-pandemii-raport-radia-zet (accessed: 22.08.2023).
Erden Ş., Elmalı Özsaray A., Deniz K.Z. (2022), Adolescents’ internet addiction, cyber bullying, and cyber victimisation in terms of various variables, “Addicta: The Turkish Journal on Addictions”, vol. 9(3), pp. 311–319.
Eurostat database. https://ec.europa.eu/eurostat/data/database
Feng Y., Ma Y., Zhong Q. (2019), The Relationship Between Adolescents’ Stress and Internet Addiction: A Mediated-Moderation Model, “Frontiers in Psychology”, no. 10, pp. 1–8. https://doi.org/10.3389/fpsyg.2019.02248
Gawrych M. (2022), Climate change and mental health: a review of current literature, “Psychiatria Polska”, vol. 56(4), pp. 903–915. https://doi.org/10.12740/PP/OnlineFirst/131991
GBD 2019. https://ghdx.healthdata.org/gbd-2019 (accessed: 10.08.2023).
GBD 2019 Mental Disorders Collaborators (2022), Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019, “Lancet Psychiatry”, no. 9, pp. 137–150.
Goto R., Pinchuk I., Kolodezhny O., Pimenova N., Skokauskas N. (2023), Study Protocol: Adolescents of Ukraine During the Russian Invasion (AUDRI) Cohort, “BMC Public Health”, no. 23: 1342. https://doi.org/10.1186/s12889-023-16070-3
Griffin J.B. Jr. (1990), Substance Abuse, [in:] Walker H.K., Hall W.D., Hurst J.W. (ed.), Clinical Methods: The History, Physical, and Laboratory Examinations, 3rd edition, Boston, Butterworths, Chapter 206. https://www.ncbi.nlm.nih.gov/books/NBK319/
Hu H., Zhang G., Yang X., Zhang H., Lei L., Wang P. (2022), Online Gaming Addiction and Depressive Symptoms Among Game Players of the Glory of the King in China: the Mediating Role of Affect Balance and the Moderating Role of Flow Experience, “International Journal Mental Health and Addiction”, no. 20, pp. 3191–3204. https://doi.org/10.1007/s11469-021-00573-4
ICD-11 for Mortality and Morbidity Statistics (Version: 01/2023), WHO, (2023). https://icd.who.int/browse11/l-m/en 17.08.20123) (accessed: 5.08.2023).
Iordache M.M., Sorici C.O., Aivaz K.A., Lupu E.C., Dumitru A., Tocia C., Dumitru E. (2023), Depression in Central and Eastern Europe: How Much It Costs? Cost of Depression in Romania, “Healthcare”, vol. 11(6), p. 921. https://doi.org/10.3390/healthcare11060921
Jeong Y.J., Suh B., Gweon G. (2020), Is smartphone addiction different from Internet addiction? comparison of addiction-risk factors among adolescents, “Behaviour & Information Technology”, vol. 39(5), pp. 578–593. https://doi.org/10.1080/0144929X.2019.1604805
Johansson A., Götestam K.G. (2004), Internet addiction: characteristics of a questionnaire and prevalence in Norwegian youth (12–18 years), “Scandinavian Journal of Psychology”, vol. 45(3), pp. 223–229. https://doi.org/10.1111/j.1467-9450.2004.00398.x
Layachi A., Schuelka M.J. (2022), The Impact of the COVID-19 related school closure on the mental health and wellbeing of children with SEN and their parents in Algeria, “International Journal of Disability, Development and Education”, vol. 71(1), pp. 24–41. https://doi.org/10.1080/1034912X.2022.2092080
Leigh J.P., Moss S.J., Sriskandarajah C. et al. (2023), A muti-informant national survey on the impact of COVID-19 on mental health symptoms of parent–child dyads in Canada, “Scientific Report”, no. 13: 7972. https://doi.org/10.1038/s41598-023-34544-7
Makaruk K., Włodarczyk J., Szredzińska R. (2020), Negatywne doświadczenia młodzieży w trakcie pandemii.[Negative experiences of young people during the pandemic], Fundacja Dajemy Dzieciom Siłę [Empowering Children Foundation].
Mental Health and COVID-19: Early evidence of the pandemic’s impact, Scientific brief, 2 March 2022, World Health Organization.
Mental health atlas 2020, (2021), World Health Organization, Geneva.
Morgül E., Kallitsoglou A., Essau C.A.E. (2020), Psychological effects of the COVID-19 lockdown on children and families in the UK, “Revista de Psicología Clínica con Niños y Adolescentes”, vol. 7(3), pp. 42–48. https://doi.org/10.21134/rpcna.2020.mon.2049
Naczelna Izba Lekarska [Supreme Medical Chamber], Zestawienie liczbowe lekarzy i lekarzy dentystów wg dziedziny i stopnia specjalizacji [Numerical summary of doctors and dentists by field and degree of specialization]. https://nil.org.pl/uploaded_files/1684479715_za-kwiecien-2023-zestawienie-nr-04.pdf (accessed: 10.05.2023).
NIK (2019), Dostępność lecznictwa psychiatrycznego dla dzieci i młodzieży (w latach 2017–2019), Informacja o wyniki kontroli [Availability of psychiatric treatment for children and adolescents (in 2017–2019), Information on inspection results], Najwyższa Izba Kontroli (NIK) [Supreme Chamber of Control], KZD.430.007.2019, Nr ewid. 170/2019/P/19/059/KZD.
Rathi M., Guha P., Neogi R. (2022), Internet addiction in adolescents: Role of family, personality and comorbid psychopathology in school children in Eastern India, “Indian Journal of Psychiatry”, vol. 64(4), pp. 408–414.
RPD (2021), Ogólnopolskie badanie jakości życia dzieci i młodzieży w Polsce, obszar nr 3: Samopoczucie psychiczne. Biuro Rzecznika Praw Dziecka [National survey of the quality of life of children and adolescents in Poland, area no. 3: Mental well-being. Office of the Ombudsman for Children], Rzecznik Praw Dziecka [Polish Ombudsmen for Children], Warsaw.
RPD (2023), Badanie jakości życia dzieci i młodzieży, perspektywa dzieci (2021) i ich rodziców [Research on the quality of life of children and adolescents, the perspective of children (2021) and their parents], Rzecznik Praw Dziecka [Polish Ombudsmen for Children], Warsaw.
Rudnik M., Wachowiak J. (2020), Uczeń z zaburzeniami psychicznymi w szkole [A student with mental disorders at school], Ośrodek Rozwoju Edukacji [Education Development Center], Warsaw.
Sharma D., Goel N.K., Sidana A., Kaura S., Sehgal M. (2023), Prevalence of Smartphone Addiction and its Relation with Depression among School-going Adolescents, “Indian Journal of Community Health”, vol. 35(1), pp. 27–31.
Shen B., Wang F., Sun S., Liu Y. (2021), Chinese Adolescents’ Academic Stress and Smartphone Addiction: A Moderated-Mediation Model, “Journal of Broadcasting & Electronic Media”, vol. 65(5), pp. 724–740. https://doi/org/10.1080/08838151.2021.2014842
Sikorska I.M., Lipp N., Wróbel P., Wyra M. (2021), Adolescent mental health and activities in the period of social isolation caused by the COVID-19 pandemic, “Advances in Psychiatry and Neurology/Postępy Psychiatrii i Neurologii”, no. 30(2), pp. 79–95. https://doi.org/10.5114/ppn.2021.108472
Sriati A., Lukman M., Agustina H.S. (2022), Relation of Academic Stress Levels and Internet Addiction in Adolescents: A Cross-Sectional Study, “Malaysian Journal of Medicine and Health Sciences”, no. 18(SUPP3), pp. 110–114.
Szredzińska R. (2022), Zdrowie psychiczne dzieci i młodzieży [Mental health of children and adolescents], pp. 136–157, [in:] Sajkowska M., Szredzińska R. (ed.), Dzieci się liczą 2022. Raport o zagrożeniach bezpieczeństwa i rozwoju dzieci w Polsce [Children matter 2022. Report on threats to the safety and development of children in Poland], Fundacja Dajemy Dzieciom Siłę [Empowering Children Foundation].
Tabak I. (2014), Zdrowie psychiczne dzieci i młodzieży. Wsparcie dzieci i młodzieży w pokonywaniu problemów [Mental health of children and adolescents. Support for children and young people in overcoming problems], “Studia BAS”, vol. 2(38), pp. 113–138.
Taufik M.H., Rezali M.S., Shahein N.A., Sahril N., Ying Ying C., Ab Wahab N.A., Kassim M.S.A. (2021), Internet Addiction and Its Associated Factors among School-going Adolescents in Malaysia, “International Journal of Public Health Research”, vol. 11(2), pp. 1466–1473.
Tayeb Z. (2021), Facebook’s own researchers found the app is bad for 360 million of its users, according to a report, November 7, 2021. https://www.businessinsider.com/facebook-papers-internal-report-app-bad-for-users-sleep-work-2021-11?IR=T (accessed: 18.08.2023).
The impact of COVID-19 on mental, neurological and substance use services: results of a rapid assessment, (2020), World Health Organization, Geneva.
Training manual for surveillance of suicide and self-harm in communities via key informants (2022), World Health Organization, Geneva.
UNICEF (2022), Global Multisectoral Operational Framework for Mental Health and Psychosocial Support of Children, Adolescents and Caregivers Across Settings, United Nations Children’s Fundation, New York.
UNICEF (2023), The global costs and benefits of mental health and psychosocial support interventions in education settings across the Humanitarian-Development Nexus, United Nations Children’s Fundation.
United Nations Youth, Definition of youth. https://www.un.org/esa/socdev/documents/youth/fact-sheets/youth-definition.pdf (accessed: 19.08.2023).
Wang Y. (2022), The Impact of Interparental Conflicts on Online Game Addiction Symptomatology: The Mediating Roles of the Parent-Adolescent Relationship and Loneliness in Adolescents, “Psychological Reports”, vol. 125(5), pp. 2337–2356. https://doi.org/10.1177/00332941211016751
WHO (2020), New WHO guidelines on promoting mental health among adolescents, World Health Organization. https://www.who.int/news/item/28-09-2020-new-who-guidelines-on-promoting-mental-health-among-adolescents (accessed: 17.08.2023).
WHO (2021a), Adolescent health, World Health Organization. https://www.who.int/health-topics/adolescent-health#tab=tab_1 (accessed: 16.08.2023).
WHO (2021b), Mental health of adolescents, World Health Organization. https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health (accessed: 18.08.2023).
WHO (2022a), Mental disorders, World Health Organization. https://www.who.int/news-room/fact-sheets/detail/mental-disorders (accessed: 17.08.2023).
WHO (2022b), Older adolescent (15 to 19 years) and young adult (20 to 24 years) mortality, World Health Organization. https://www.who.int/news-room/fact-sheets/detail/levels-and-trends-in-older-adolescent-(15-to-19-years)-and-young-adult-(20-to-24-years)-mortality (accessed: 17.08.2023).
WHO Factsheet for World Mental Health Day 2018, (2018), Regional Office for Europe. https://www.who.int/mental_health/world-mental-health-day/2018/en/ (accessed: 2.11.2019).
Wolf J., Prüss-Ustün A., Ivanov I., Mugdal S., Corvalán C., Bos R., Neira M. (2018), Preventing disease through a healthier and safer workplace, Geneva, World Health Organization. https://www.who.int/quantifying_ehimpacts/publications/healthier-workplace/en/ (accessed: 2.11.2019).
World mental health report: transforming mental health for all, (2022), World Health Organization, Geneva.
Yang S.C., Tung C. (2007), Comparison of Internet addicts and non-addicts in Taiwanese high school, “Computers in Human Behavior”, vol. 23(1), pp. 79–96.
Yılmaz A.Y., Aydoğdu F., Koçtürk N. (2022), A Systematic Overview of Adolescents’ Smartphone Habits and Internet Addiction During the COVID-19 Era, “Psikiyatride Güncel Yaklaşımlar-Current Approaches in Psychiatry”, vol. 14(4), pp. 510–517. https://doi.org/10.18863/pgy.1064501
Abstrakt. Rozpowszechnienie zaburzeń psychicznych w populacji gwałtownie rośnie w ostatnich latach, a młodzi ludzie są grupą szczególnie wrażliwą. Są nie tylko bardziej narażeni na zaburzenia psychiczne, ale dochodzi również do trwającej długi czas kumulacji obciążeń. Obecnie skala problemu jest ogromna. W związku z tym różne organizacje i zrzeszenia ostrzegają w związku z trwającym kryzysem zdrowia psychicznego.
Niniejsze badanie ma na celu zbadanie skali kryzysu zdrowia psychicznego młodzieży w kontekście rozwoju społeczno-gospodarczego. Skupiono się na związanych z tym problemem obciążeniach dla społeczeństwa i gospodarki, a także na dostrzeganych postępach w zakresie podstawowych problemów. Ocena tego zjawiska jest dokonywana poprzez studia literaturowe i eksploracyjną analizę danych, które pozwalają na wskazanie bieżących tendencji i nowych zjawisk dotyczących czynników ryzyka i zaburzeń psychicznych młodych ludzi, zarówno globalnie, jak i koncentrując się na polskiej perspektywie, a ponadto ocenę dostępności psychiatrycznej opieki zdrowotnej w Polsce, Europie i na świecie.
Uzyskane wyniki wskazują, że zdrowie psychiczne i dobrostan psychiczny przez długi czas nie były uznawane za priorytety opieki zdrowotnej. W szczególności trzy kwestie zasługują na szczególną uwagę w kontekście kryzysu zdrowia psychicznego młodzieży. Po pierwsze, uzależnienia, zwłaszcza od Internetu i smartfonów, co staje się globalnym problemem wśród młodych ludzi. Po drugie, wpływ pandemii COVID-19 odpowiadającej za katastrofalny stan zdrowia psychicznego dzieci i młodzieży. Po trzecie, dostępna opieka psychiatryczna i jej jakość są nieadekwatne do rosnących potrzeb młodych ludzi we współczesnym świecie.
Słowa kluczowe: zdrowie psychiczne młodzieży, zaburzenia psychiczne, uzależnienia, społeczne obciążenie zaburzeniami psychicznymi, ekonomika zdrowia, zdrowie psychiczne młodzieży w Polsce, psychiatryczna opieka zdrowotna, rozwój społeczno-gospodarczy, badania regionalne

