Available online at: https://doi.org/10.18778/1898-6773.87.3.05
 https://orcid.org/0000-0001-8375-8818
https://orcid.org/0000-0001-8375-8818
University of Warsaw, Faculty of Archaeology, Poland
 https://orcid.org/0000-0002-6043-8472
https://orcid.org/0000-0002-6043-8472
University of Bialystok, Faculty of International Relations, Poland
ABSTRACT: This study investigates the etiology of a bifid mandibular condyle found in a Bogaczewo culture cremation burial from the Paprotki Kolonia site 1. Using macroscopic analysis and CT imaging, we identified a sagittal separation of the mandibular condyle, suggesting a developmental origin. This represents the first known case of a bifid mandibular condyle from an Iron Age cremation context. Analytical potential is limited due to the preservation of only one condyle and the absence of teeth and temporobandibular surface, which do not allow us to assess the impact of this condition to the life quality of the individual.
KEY WORDS: cremated human remains, bone malformation, Iron Age, Bogaczewo Culture.
Multi-headed mandibular condyles are often incidentally detected during radiographic examinations in both adults and children (Artvinil and Kansu 2003; Ertas et al. 2013; Jha et al. 2013). Proposed etiologies for these abnormalities include malformations during early childhood development (Blackwood 1957; Ertas et al. 2013), hindrance in blood supply (Hrdlička 1941), and childhood trauma (Cowan and Ferguson 1997; Daniels and Ali 2005). However, these lesions are often classified as non-specific, lacking a known etiology (Almăşan et al. 2011; Antoniades et al. 2004; Cowan and Ferguson 1997; Dennison et al. 2008; Ertas et al. 2013; Espinosa-Femenia et al. 2006; Moraes Ramos et al. 2006; Szentpétery et al. 1990). The earliest known report of a bifid mandibular condyle (BMC) dates back to the Late Neolithic period (Williams and Polet 2017).
This study introduces the case of BMC obtained from an archaeological cremation burial of Bogaczewo culture. We provide a description of this condition, a differential diagnosis, and considerations regarding its etiology. This report contributes to the understanding of populational occurrence of multi-headed mandibular condyles from archaeological contexts, particularly in the context of cremation burials and the potential diagnosis of this paleopathology in burned human remains.
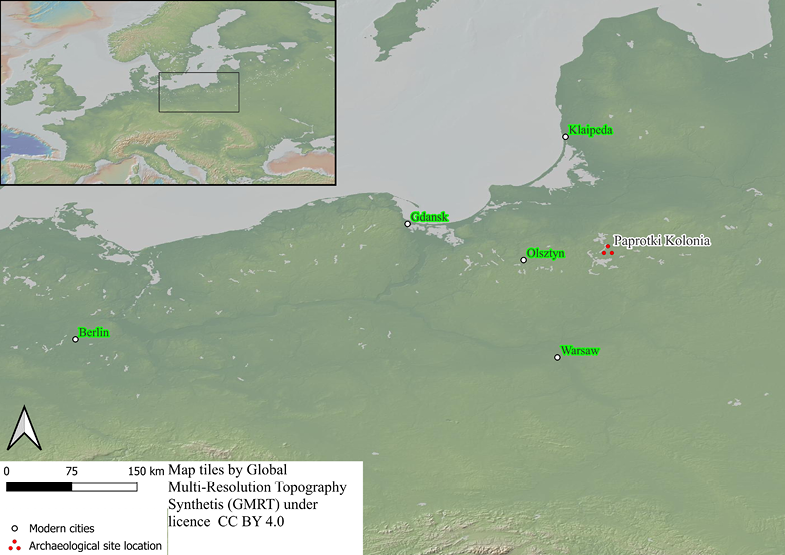
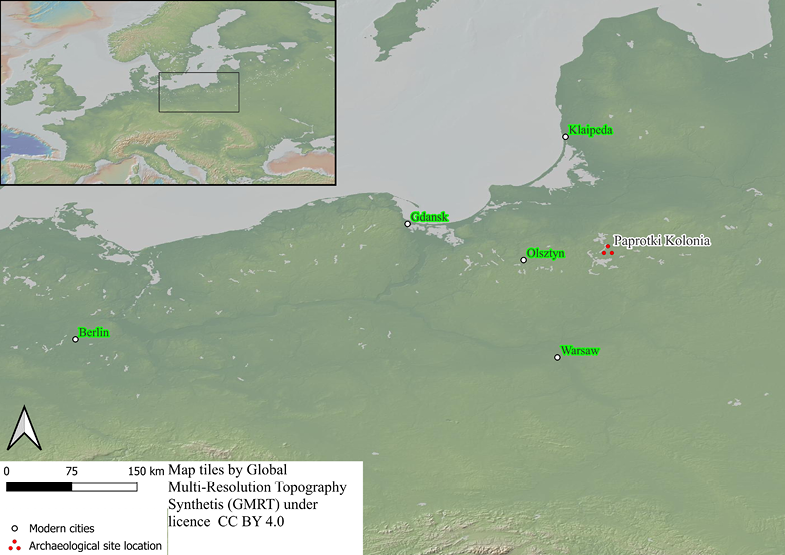
Fig. 1. Geographic location of Paprotki Kolonia site 1. Selected large modern cities marked as the reference
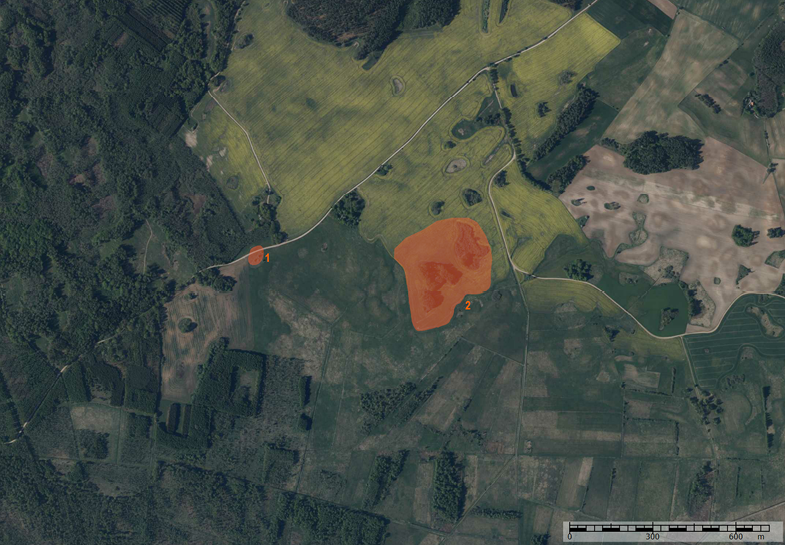
Fig. 2. The present-day landscape of the north shore of the former Lake Wons with the location of relics of the cemetery (1) and associated settlement (2)
The cemetery in the village of Paprotki Kolonia is situated in the Mazurian Lakeland, northeastern Poland (Fig. 1). So far, 539 human graves, 11 offering pits with horse skeletons, and relics of pyres were discovered there. The cemetery is dated from the 1st until the 6th century A.D. All human graves were cremation graves in clay urns or without, usually with the charcoals from the pyre inside the grave pit. Urns exhibited stylistic diversity in terms of form, ornamentation, and metric features. Currently, studies of burials from Bogaczewo culture cemeteries, including Paprotki Kolonia cemetery (French et al. 2024; Karczewski 2011), Łężany (Wiśniewska 2014), and Samławki VII (Budziszewski 2018) reported that while graves with Minimum Number of Individuals (MNI)=1 are the predominant burial form, the occurrence of burials with MNI>1 was confirmed in all bioarchaeologically studied Bogaczewo culture cemeteries. In this category of burials, it is more common for an adult to be buried together with a non-adult. However, graves containing the remains of two or more adults are also known.
However, no clear relationship was found between the MNI and the funerary urn’s form, ornamentation or dimensions. Some of the burials with MNI=1 have larger dimensions than urn burials with MNI>1 (Karczewski 2011; Wiśniewska 2014). This cemetery belongs to the so-called Bogaczewo Culture, an archaeological equivalent for part of the West Balts community in the 1st half of the 1st millennium A.D. Material traces of the funeral rite do not indicate the existence of lasting social differentiation of the community using the cemetery. No graves have been discovered that differed from the others in terms of particularly rich equipment or a different form of burial. Weapon elements discovered in men’s graves, such as spearheads, combat knives, shield elements indicate that these were warrior burials. The vertical and horizontal stratigraphy of individual grave clusters indicate that subsequent graves were arranged around the chronologically oldest grave located in the center of grouping. This focal grave usually contained the burned remains of an adult male suggesting a patrilineal structure of the community. The remains of plants and animals discovered in graves were used as elements of the funeral ritual. Such remains were also found in the relics of the settlement whose people used the cemetery (Fig. 2), which proves that it was an agricultural community. Their additional activities included fishing, hunting and gathering. The non-agricultural activities included ferrous and non-ferrous metallurgy, weaving, bone, antler, and amber processing, as well as pottery making.
The grave No. 75 was located in the west part of the cemetery, on the north edge of the large cluster of graves (Fig. 3). It had stratigraphic relations with graves No. 85 and 102. It was a large urn cremation burial with no relics of pyre, excavated during the field season 1992. Insite the urn, between fragments of burnt human bones, an amber bead and a miniature clay vessel were found. All graves – No. 75, 85, and 102 were dated to phases C2-D (ca. 260-450 A.D.).
Fig. 3. A fragment of the plan of the western part of the cemetery with the location of grave no. 75 marked by red color. Trenches from World War I marked with gray color
The cremation burial was analyzed with the methodological protocol proposed by Jacqueline McKinley (1994) and recently by Elżbieta Jaskulska (2020) with the use of a set of three calibrated sieves. It allowed us to describe and determine the biological profile and cremation burial practices in the case of the single urn burial 75. The sex of individuals was assessed based on the morphology of skull fragments and pelvic morphology (Acsádi and Nemeskéri 1970 cited in Buikstra and Ubelaker 1994; Phenice 1969). Furthermore, the general morphology of preserved bone fragments in terms of robusticity and gracility was taken into account, based on the observation of Jacqueline McKinley (1994:6).
Age-at-death was assessed based on the development of long bones and the axial skeleton (Cunningham et al. 2016), and cranial suture obliteration (Meindl and Lovejoy 1985).
A total of 1837.9 grams of human cremains were deposited in the analyzed urn. The cremains of two adult individuals have been identified in burial 75 based on the presence of two right zygomatic processes of the frontal bone, two right mandibular condyles, and two left frontal processes of the zygomatic bone. Bone fragments also exhibit a visible diversity in size, especially in the case of mandibular condyles. The mediolateral dimension of the first right mandibular condyle (a) is 250 mm, and the second right mandibular condyle (b) is 150 mm. The presence of a male individual (Acsádi and Nemeskéri 1970 cited in Buikstra and Ubelaker 1994) was assessed based on the presence of a pronounced right supraorbital margin (score=5), and nuchal lines of the occipital bone (score=4). This was also confirmed by a preserved right greater sciatic notch (score=4, Phenice 1969). Finally, the general morphology of the bone fragments indicates visible differences in robusticity between a male and a second individual interred in the discussed burial. The presence of a female individual was additionally confirmed and assessed based on the presence of gracile bone fragments and preserved left supraorbital margin (score=2), right mastoid process (score=1), and glabella (score=2). Based on the measurements, the malformed mandibular condyle was assigned to the male individual. Among these 1837.9 g of human cremains, there was not a single bone fragment indicating a distinctly different degree of development of the human osseous system, and significant number of cranial bones with obliteration of sutures in the endocranial surface making it unreasonable to conclude that a non-adult individual was deposited in this burial.
A deep and oval groove is present in the middle of the BMC, separating it into two, nearly equal in size heads in the sagittal plane (Fig. 4a, 4b). The pitting is visible within the mentioned medial groove. Lateral and medial views of the affected mandibular condyle present the morphology of the groove and its depth in the additional perspectives (Fig. 4c, 4d). The maximum mediolateral diameter of the groove is 3 mm and the maximum anterioposterior diameter of the groove is 8 mm This lesion caused the characteristic Y-shaped BMC (Fig. 4e). No osteophytes, tumors, or alternations on the articular surfaces have been observed on the BMC.
CT image of the BMC under discussion presents the normal cancellous bone presence without any signs of remodelling, fracture lines or bone microstructural disturbances (Fig. 5a, Fig. 5b, Fig. 5c, Fig. 5d). Furthermore, these images offer additional documentation of the BMC’s morphology, confirming the symmetrical sagittal condyle separation by a curved groove.
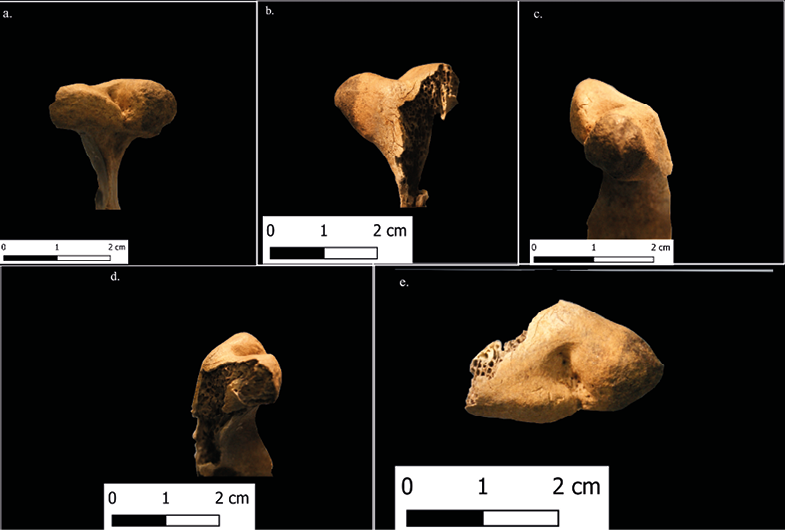
Fig. 4. BMC from the funerary urn 75 from Paprotki Kolonia site 1. A. The mandibular condyle from the anterior view. B. posterior view. C. medial view. D. lateral view. E. superior view
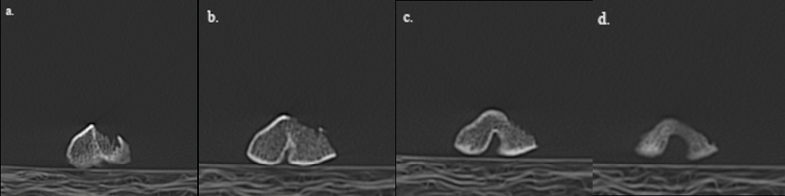
Fig. 5. Series of CT scan images of BMC (a–d), displaying a series of cross sections through the condyle for the visualization of internal bone structure
Bifid and multi-headed mandibular condyles are considered rare conditions and are often described as developmental traits with an unknown etiology (Hrdlička 1941). Publications addressing these lesions in archaeological contexts frequently rely on clinical medical reports and echo the etiological conclusions drawn therein. The following section provides observations grounded in the most frequently cited symptoms found in the literature to establish the etiology of the discussed lesion (Table 1).
Among the various etiological mechanisms proposed for the BMC, the case from Paprotki Kolonia aligns most closely with developmental or trauma-induced instances. The absence of osteoarthritic changes, osteophytes, osteochondroma, and lobulation on the condyle surface justifies the exclusion of degenerative or tumor etiology.
Currently, trauma is the most frequently cited etiological mechanism of the BMC in the clinical literature (Antoniades et al. 2004; Cornwall et al. 2015; Cowan and Ferguson 1997; Daniels and Ali 2005; Ertas et al. 2013; González-Garrido et al. 2020; Güven 2018). Szentpétery et al. (1990) were the first to suggest a distinction between sagittal separation of the condyle because of traumatic etiology and coronal separation as characteristics of developmental origin. However, cases of coronal separation of the condyle with confirmed trauma record were also reported in multiple studies (Almăşan et al. 2011; Cowan and Ferguson 1997; Daniels and Ali 2005; Lund 1974; Hersek et al. 2004; Shriki et al. 2005). Moreover, sagittal separation, both unilateral and bilateral, is often recorded in individuals with no known history of trauma (Antoniades et al. 1993; Cornwall et al. 2015; Cowan and Ferguson 1997; Daniels and Ali 2005; Güven 2018; Hersek et al. 2004; Jordana et al. 2004; Kahl et al. 1995; Loh and Yeo 1990). Severe trauma cases in clinical records involve condylar dislocation or dysplasia accompanied by flattening of the mandibular condyle, osteoarthritic changes, and temporomandibular joint (TMJ) ankylosis (Cornwall et al. 2015; Daniels & Ali 2005; Güven 2018).
Clinical records often associate BMC with symptoms such as trismus, clicking, deviation toward the affected side, and pain during mouth opening, although this condition does not consistently hinder TMJ motion or functionality (Almăşan et al. 2011; Ertas et al. 2013; Espinosa-Femenia et al. 2006; Gundlach et al. 1987; Hersek et al. 2004; Loh and Yeo 1990; Lysell and Öberg 1975). Conversely, post-traumatic cases of bifid and trifid mandibular condyles often result in significant restriction of joint functionality and movement (Jha et al. 2013; Moraes Ramos et al., 2006), particularly when osteoarthritis accompanies BMC (Rando and Waldron 2012). Further progression of degenerative lesions can gradually decrease the ability to open the mouth (Antonidades et al. 2004; Cowan and Ferguson 1997; Daniels and Ali 2005; Espinosa-Femenia et al. 2006; Hersek et al. 2004). This can hinder food consumption or create discomfort during eating, especially when biting harder foods. In severe cases, particularly those associated with dislocation of the mandibular condyle and fracture of the condylar neck, these injuries may lead to visible facial asymmetry (Dimitroulis 1997; Ertas et al. 2013; Hersek et al. 2004; Kahl et al. 1995; Shriki et al. 2005; Zachariades et al. 2006). On the other hand, non-traumatic cases of BMC are commonly not associated with any symptoms or incidents of moderate pain and clicking during the activity of TMJ (Almăşan et al. 2011; Daniels and Ali 2005).
| Symptom | BMC from Paprotki Kolonia | Childhood trauma | Adulthood trauma | Developemental origin | Degenerative conditions | Tumor |
| Osteoarthritis | - | - | +a, d, e | - | +g | - |
| Medial groove | + | +a, b, c | +a, e | +a, c, e | - | - |
| Flattening of mandibular condyle | - | - | +a, e | - | - | - |
| Lobulation of manidublar condyle | - | - | - | - | +g | + |
| Signs of bone healing | - | +a | +a, d, e | - | +g | - |
| Condyle dislocation | - | - | +a | - | - | - |
| Sagittal separation of mandibular condyle | + | +a, b | +a, d, e | +a, c, e | - | - |
| Coronal separation of mandibular condyle | - | +a, b, c | - | +c, e | - | - |
| Osteochondroma | - | - | - | - | - | +h, i |
| Ankylosis | - | +a, b | +a, e | - | +g | - |
| Separated mandibular fossa | - | - | - | - | - | - |
| Condylar neck separatation | - | - | +a, d, e | - | - | - |
+ Lesions consistent with condition.
- Lesions inconsistent with condition.
a Cowan, D.F., Ferguson, M.M., 1997. “Bifid mandibular condyle”. Dentomaxillofac. Radiol. 26, 70–73.
b Daniels, J.S.M., Ali, I. 2005. “Post-traumatic bifid condyle associated with temporomandibular joint ankylosis: Report of a case and review of the literature”. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology, 99(6), 682–688.
c Blackwood, H.J.J., 1957. „The Double-Headed Mandibular Condyle”. American Journal of Physical Anthropology 15 (1): 1–8.
d Dennison, J., Mahoney, P., Herbison, P., & Dias, G., 2008. „The False and the True Bifid Condyles”. HOMO 59 (2): 149–59.
e Szentpétery, A., Kocsis, G., & Marcsik, A. 1990. “The problem of the bifid mandibular condyle”. Journal of Oral and Maxillofacial Surgery, 48(12)
g Açikgöz, A. 2006. “Bilateral bifid mandibular condyle: A case report”. Journal of Oral Rehabilitation, 33(10), 784–787.
h González-Garrido, L., Gómez-González, S., Gonzalo-Orden, J.M., & Wasterlain, S.N., 2022. „Multi-headed (bifid and trifid) mandibular condyles in archaeological contexts: Two posttraumatic cases”. Archives of Oral Biology 134: 105326.
i Hersek, N., Özbek, M., Taşar, F., Akpınar, E., Fırat, M., 2004. „Bifid Mandibular Condyle: A Case Report”. Dental Traumatology 20 (3): 184–186.
Despite the increasing number of recorded cases of BMC in both archaeological and medical contexts, its etiology remains poorly understood (Dennison et al. 2008; Loh and Yeo 1990; Moraes Ramos et al. 2006). In the discussed case, the fragmentation caused by the cremation process hampers our ability to precisely estimate the impact of BMC on the individual’s quality of life. However, based on both macroscopic features and radiographic depiction, we suggest that this variation is of developmental origin, most similar to the Blackwood (1957) theory of the early development disturbance in the condylar cartilage, due to the lack of any macroscopic or radiographic signs of bone healing or remodeling of bone structure, which would indicate traumatic origin (Cowan and Ferguson 1997; Loh and Yeo 1990).
This report thus presents another early example of BMC, from Central Europe, dating back to the Iron Age. Moreover, to our knowledge, this is the first reported case of BMC from a prehistoric cremation burial.
Ethics statement
The research procedures undertaken during the analysis published in this report were performed following the BABAO Codes of Ethics and Practice. This article has not been previously published or concurrently submitted to an editorial office of another journal, and it is approved by all authors and the institutions.
Data availability statement
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study
Acknowledgements
We would like to thank Dr. Hanna Mankowska-Pliszka for her help with conducting the computed tomography.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of interest:
none.
Authors’ contribution
AB was responsible for conceptualization, methodology, formal analysis, writing the original draft, review and editing, and visualization. MK was responsible for data curation, investigation, providing resources, writing the original draft, and review and editing.
Açikgöz A. 2006. Bilateral bifid mandibular condyle: A case report. Rom J Oral Rehabil 33(10):784–787. https://doi.org/10.1111/j.1365-2842.2005.01595.x
Almăşan OC, Hedeşiu M, Băciuț G, Băciuț M, Bran S, Jacobs R. 2011. Nontraumatic Bilateral Bifid Condyle and Intermittent Joint Lock: A Case Report and Literature Review. J Oral Maxillofac Surg 69(8):e297–e303. https://doi.org/10.1016/j.joms.2011.03.072
Antoniades K, Hadjipetrou L, Antoniades V, Paraskevopoulos K. 2004. Bilateral bifid mandibular condyle. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 97(4):535–538. https://doi.org/10.1016/j.tripleo.2003.09.003
Antoniades K, Karakasis D, Elephtheriades J. 1993. Bifid mandibular condyle resulting from a sagittal fracture of the condylar head. Br J Oral Maxillofac Surg 31(2):124–126. https://doi.org/10.1016/0266-4356(93)90176-W
Blackwood HJJ. 1957. The double-headed mandibular condyle. Am J Phys Anthropol 15(1):1–8. https://doi.org/10.1002/ajpa.1330150108
Budziszewski A. 2018. Diversity of Cremation Mortuary Rites Reconstructed Using Fragmentation Pattern at the Multicultural Cemetery Samławki VIII, Poland [M.A. Thesis]. University of Warsaw.
Cornwall J, Samarakoon L, Antony DJ, Dias GJ. 2015. Morphological and degenerative changes in a suspected post-traumatic bifid mandibular condyle. Anatomy 8(1):27–33. https://doi.org/10.2399/ana.14.042
Cowan DF, Ferguson MM. 1997. Bifid mandibular condyle. Dentomaxillofacial Radiology 26(1):70–73. https://doi.org/10.1038/sj.dmfr.4600214
Cunningham C, Scheuer L, Black S. 2016. Developmental Juvenile Osteology. London: Academic Press.
Daniels JSM, Ali I. 2005. Post-traumatic bifid condyle associated with temporomandibular joint ankylosis: Report of a case and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 99(6):682–688. https://doi.org/10.1016/j.tripleo.2004.11.051
Dennison J, Mahoney P, Herbison P, Dias G. 2008. The false and the true bifid condyles. HOMO 59(2):149–159. https://doi.org/10.1016/j.jchb.2008.02.001
Dimitroulis G. 1997. Condylar injuries in growing patients. Aust Dent J 42(6):367–371. https://doi.org/10.1111/j.1834-7819.1997.tb06079.x
Ertas ET, Sahman H, Yircali Atici M. 2013. Bilateral bifid mandibular condyle: Report of a case with condylar fractures. J Oral Maxillofac Radiol 1(2):80–82. https://doi.org/10.4103/2321-3841.120127
Espinosa-Femenia M, Sartorres-Nieto M, Berini-Aytés L, Gay-Escoda C. 2006. Bilateral Bifid Mandibular Condyle: Case Report and Literature Review. Cranio 24(2):137–140. https://doi.org/10.1179/crn.2006.021
French KM, Musiał AD, Karczewski M, Daugnora L, Shiroukhov R, Ropka-Molik K, et al. 2024. Biomolecular Evidence Reveals Mares and Long-Distance Imported Horses Sacrificed by the Last Pagans in Temperate Europe. Science Advances 10(20):eado3529. https://doi.org/10.1126/sciadv.ado3529
González-Garrido L, Gómez-González S, Gonzalo-Orden JM, Wasterlain SN. 2022. Multi-headed (bifid and trifid) mandibular condyles in archaeological contexts: Two posttraumatic cases. Arch Oral Biol 134:105326. https://doi.org/10.1016/j.archoralbio.2021.105326
Gundlach KKH, Fuhrmann A, Ven G. 1987. The double-headed mandibular condyle. Oral Surgery, Oral Medicine, Oral Pathology 64(2):249–251. https://doi.org/10.1016/0030-4220(87)90098-3
Güven O. 2018. A study on etiopathogenesis and clinical features of multi-headed (bifid and trifid) mandibular condyles and review of the literature. J Craniomaxillofac Surg 46(5):773–778. https://doi.org/10.1016/j.jcms.2018.02.011
Hersek N, Özbek M, Taşar F, Akpınar E, Fırat M. 2004. Bifid mandibular condyle: A case report. Dental Traumatology 20(3):184–186. https://doi.org/10.1111/j.1600-4469.2004.00222.x
Hrdlička A. 1941. Lower jaw: Double condyles. Am J Phys Anthropol 28(1):75–89. https://doi.org/10.1002/ajpa.1330280104
Jaskulska E. 2020. Analysis of Human Cremains. University of Warsaw.
Jha A, Khalid M, Sahoo B. 2013. Posttraumatic Bifid and Trifid Mandibular Condyle With Bilateral Temporomandibular Joint Ankylosis. J Craniofac Surg 24(2):166. https://doi.org/10.1097/SCS.0b013e31827c83cd
Jordana X, García C, Palacios M, Chimenos E, Malgosa A. 2004. Bifid mandibular condyle: Archaeological case report of a rare anomaly. Dentomaxillofacial Radiology 33(4):278–281. https://doi.org/10.1259/dmfr/16519922
Karczewska M, Karczewski M. 2016. Landscapes of Cemeteries from the Roman and Migration periods in the Masurian Lakeland (Northeast Poland). Archaeologia Baltica 23:96–111.
Karczewski M. 2011. Archeologia środowiska zachodniobałtyjskiego kręgu kulturowego na pojezierzach. Białystok: Bogucki Wydawnictwo Naukowe.
Loh FC, Yeo JF. 1990. Bifid mandibular condyle. Oral Surgery, Oral Medicine, Oral Pathology 69(1):24–27. https://doi.org/10.1016/0030-4220(90)90263-R
Lund K. 1974. Mandibular growth and remodelling process after condylar fracture. A longitudinal roentogence-phalometric study. Acta Odontologica Scandinavica. Suppl. 32(64):1–114.
Lysell G, Öberg T. 1975. Unilateral Doubling of Mandibular Condyle. Dentomaxillofacial Radiology 4(2):95–98. https://doi.org/10.1259/dmfr.1975.0059
McKinley J. 1994. The Anglo-Saxon Cemetery at Spong Hill, North Elmham, Part VIII: The Cremations. Norfolk: East Anglian Archaeology. Available at: http://eaareports.org.uk/publication/report69/
Meindl RS, Lovejoy CO. 1985. Ectocranial suture closure: A revised method for the determination of skeletal age at death based on the lateral-anterior sutures. Am J Phys Anthropol 68(1):57–66. https://doi.org/10.1002/ajpa.1330680106
Moraes Ramos FM, Filho JO de V, Manzi FR, Bóscolo FN, Almeida SM. 2006. Bifid mandibular condyle: A case report. J Oral Sci 48(1):35–37. https://doi.org/10.2334/josnusd.48.35
Phenice TW. 1969. A newly developed visual method of sexing the os pubis. American Am J Phys Anthropol 30(2):297–301. https://doi.org/10.1002/ajpa.1330300214
Rando C, Waldron T. 2012. TMJ osteoarthritis: A new approach to diagnosis. Am J Phys Anthropol 148(1):45–53. https://doi.org/10.1002/ajpa.22039
Shriki J, Lev R, Wong BF, Sundine MJ, Hasso AN. 2005. Bifid mandibular condyle: CT and MR imaging appearance in two patients: Case report and review of the literature. Am J Neuroradiol 26(7):1865–1868.
Szentpétery A, Kocsis G, Marcsik A. 1990. The problem of the bifid mandibular condyle. J Oral Maxillofac Surg 48(12):1254–1257. https://doi.org/10.1016/0278-2391(90)90477-J
Williams FL, Polet C. 2017. A secondary mandibular condylar articulation and collateral effects on a Late Neolithic mandible from Bois Madame rockshelter in Arbre, Belgium. Int J Paleopathol 16:44–49. https://doi.org/10.1016/j.ijpp.2016.12.003
Wiśniewska A. 2014. Łężany: Cmentarzysko z okresu wpływów rzymskich i wędrówek ludów na Pojezierzu Mrągowskim. Badania w sezonie 2013. Warsaw: Fundacja Dajna im. Jerzego Okulicza-Kozaryna.
Zachariades N, Mezitis M, Mourouzis C, Papadakis D, Spanou A. 2006. Fractures of the mandibular condyle: A review of 466 cases. Literature review, reflections on treatment and proposals. J Craniomaxillofac Surg 34(7):421–432. https://doi.org/10.1016/j.jcms.2006.07.854

