Introduction
The necropolis of the Pozzanghera district (contrada), located near Lentini (the ancient Greek town of Leontinoi, Λεοντῖνοι, home to the famed sophist Gorgias, 483–375 BC) in the present archaeological area in the province of Syracuse in eastern Sicily (Fig. 1), was subjected to systematic archaeological excavations between 26th October 1981 and 9th January 1982. The investigations were led by Prof. Dario Palermo (Full Professor of archaeology at the University of Catania and co-author of this article) and carried out in close collaboration with the Superintendency of Syracuse. The chronology of the site is very broad: the oldest tombs (Tombs 37 and 38) date to the Final Bronze Age (11th–9th centuries BC), therefore before the arrival of Greek settlers. Subsequently the Pozzanghera area was reutilised again as a necropolis starting from the 6th century BC (Tomb 48), while all the other burials date to a period comprised between the 5th and 4th centuries BC. At the end of the last excavation campaign 55 burials were brought to light (Palermo 1991). Among these, Tomb 32 from Trench 7 (Fig. 2), which is the main focus of the present analysis, is bioarchaeologically relevant because of a vertebral anomaly detected in the skeleton found in this burial (Melintenda 2021), which will be discussed here.
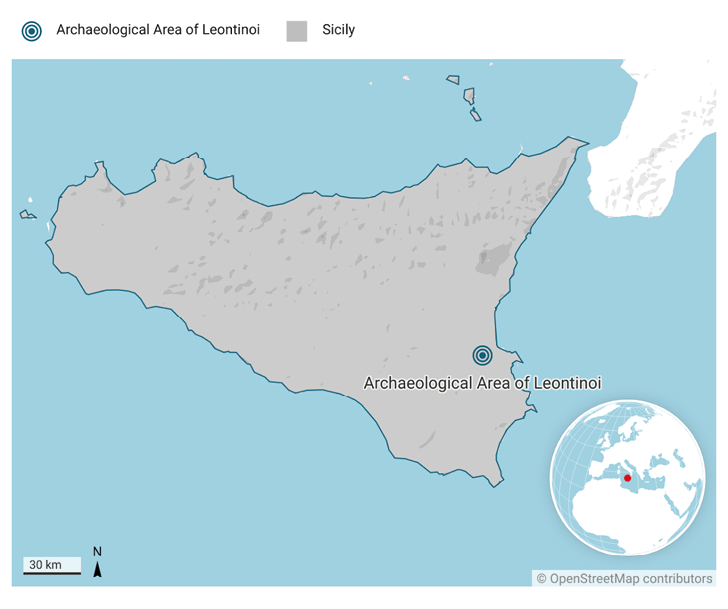
Fig. 1. Location of the Pozzanghera necropolis inside the Archaeological Area of Leontinoi
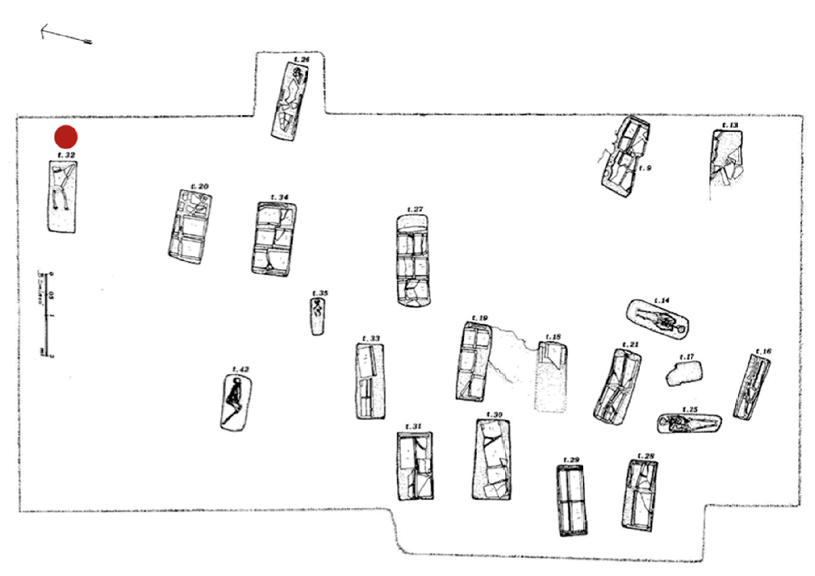
Fig. 2. Map of the Burials, Trench 7, from Palermo 1991. The red dot indicated the position of Tomb 32
Materials and Methods
The quantitative and qualitative analysis of the state of preservation were calculated by means of the Bello indices (2001): Bone Representation Index (B.R.I.) expressed as the ratio between the number of found bones and the theoretical number of bones that should be present in the actual total palaeodemography derived from the number of individuals retrieved in anatomical connection; Anatomical Preservation Index (A.P.I.) expressed as the ratio of conservation scores (in percentage) attributed to each bony element which constitutes the skeleton and the total number of bones of the skeleton (Bello 2001). The quality of the preservation of the cortical surfaces was evaluated through the Qualitative Bone Index (Q.B.I.), expressed as the ratio between the fully preserved cortical surfaces and the damaged ones for each skeletal segment (Bello 2001).
The sex of the individual was determined through the analysis of the morphological features of the retrieved fragments of the skull and pelvis (Ferembach et al. 1977–1979). Estimation of the individual’s age at death was performed through the analysis of dental wear (Lovejoy 1985) and morphological changes of the auricular surface of the ilium (Lovejoy et al. 1985). Measurements of the sacral fragment’s anomaly were taken using a digital sliding caliper.
The palaeopathological analysis was carried out by adopting a morphological, descriptive and metrical approach (Aufderheide and Rodríguez-Martín 2005; Ortner 2019; Varotto et al. 2021) and comparing the case with similar ones published in the specialised literature (Henneberg and Henneberg 1999). The sacral fragment was additionally subjected to radiological investigation. X-ray machine: Villa – Apollo EZ; X-ray parameters: 50kV 16mAs; CT scan machine: Siemens Somatom Sensation 16; CT scan parameters: 140kV 280mAs. A 3D reconstruction of the sacral fragment was performed using the OsiriX MD version 13.0.1 (Pixmeo).
Moreover, in order to chronologically contextualise the present palaeopathological report, a literature search was carried out on the free search engines PubMed, Google Scholar, Wiley Online Library, complemented by a Google and Google Books (English and Italian versions) search, using combinations of the following keywords: “spina bifida”, “spina bifida occulta”, “vertebral anomalies”, “spine congenital disease”, “neural tube defects” AND “Sicily”, “Sicilian” AND “archaelogy”, “anthropology”, “bioarchaeology”, “palaeopathology”, “paleopathology”, “archaeology”, in order to identify publications that may help to reconstruct a chronological sequence of published reports of this condition in the bioarchaeological and palaeopathological record of Sicily. The main goal of this search was not making a comprehensive review of spina bifida in Sicily, but to verify if mentions of it existed in the specialised literature for the centuries before Christ, hence in a time frame including the chronology of Pozzanghera necropolis. In this search, non-indexed and non-bibliometric Italian-language archaeological sources were not included.
Results
At the time of its excavation, the skeleton found in Tomb 32 lay in the supine position, with a bronze needle and a small 5th century BC λήκυθος /lékythos/ (a narrow-necked flask used in antiquity as a container for oils and ointments) next to the skull (Palermo 1991, Fig. 3). The preservation of the skeletal districts is partial. As far as the preservation indexes are concerned, they are as follows:
- B.R.I. = 35% (poor representation),
- A.P.I. = 50% (fairly good anatomical preservation),
- Q.B.I. = 47% (modest quality of the bone surface).
The individual’s sex was determined to be male based on the morphologies of the external occipital protuberance and the mastoid processes at the cranial level and, in the pelvis, on the absence of the preauricular sulcus. As for the individual’s age at the moment of death it was estimated to be of 24–30 years, hence a young adult based on dental wear, and 25–29 years (Phase 2) based on the morphology of the auricular surface of the ilium.
The sacrum is severely incomplete: only a small portion of it belonging to the first sacral vertebra and from the third to the fifth sacral vertebra have preserved to this day (Fig. 4). This more caudally preserved sacral segment is affected by an evident lack of closure of the neural arch at S3 – hence cranially to S4 where the sacral canal usually terminates with the sacral hiatus – to a presentation whose morphology is thus compatible with spina bifida occulta. Of note, this case of spina bifida is not only represented by the presence of the groove created by the lack of fusion of the posterior vertebral arches, but it also shows a considerable distance between the two edges of the neural arches.
The following measures of the patent sacral canal (S3–S5) are provided:
- Maximum length of the open sacral canal: 32.3 mm
- Maximum width of the open sacral canal: 19.5 mm.
These features are also palaeoradiologically observed (Fig. 5a–d), with the possibility, especially through CT transverse sections (Fig. 5b,c) to explore, in a cranio-caudal direction, how the posterior vertebral neural arch widens up to a complete separation creating the investigated dysraphism.
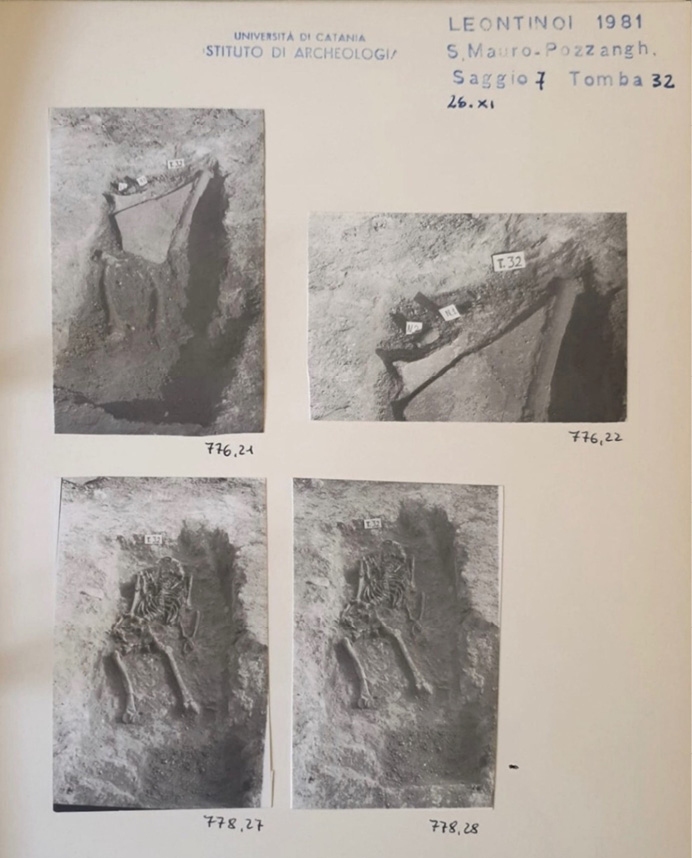
Fig. 3. Tomb 32 at the moment of its complete excavation. Photos from Dario Palermo’s personal archive

Fig. 4. Dorsal view of the fragment of the sacrum from Tomb 32 with spina bifida sacralis occulta
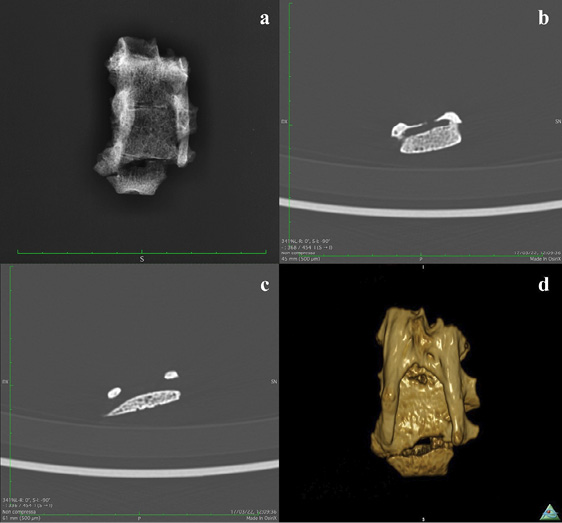
Fig. 5.a. X-ray image of the sacral fragment in postero-anterior projection
Fig. 5.b. CT scan image (transverse section) at the origin of the dysraphism (S3)
Fig. 5.c. CT scan image (transverse section) at a more caudal level (S4), well within the sacral hiatus
Fig. 5.d. 3D virtual reconstruction of the sacral fragment with spina bifida in dorsal view
Discussion
This condition occurs when an incomplete bone line appears on one or more neural arches. It is found in the lumbosacral region, most frequently in the sacrum (spina bifida sacralis). Spina bifida can occur in two different variants, occulta (SBO) and aperta (SBA) (Aufderheide and Rodríguez-Martín 1998). SBO consists of an incomplete fusion of the posterior neural arch and may affect one or more sacral segments. SBO can involve one or two vertebrae: in particular, the first sacral vertebra is statistically the most affected one, as highlighted by studies on living patients such as the review of 1,200 radiological images of Israeli patients which showed that 17% of them had that specific anatomical location (S1) (Nastoulis et al. 2019). The meninges do not protrude outside of this defect. Thus, spina bifida occulta can be diagnosed radiologically in living patients, often not earlier than late childhood or adulthood as it may well lead to no relevant disabilities. Nonetheless, in the number of reported clinical consequences of SBO the cutaneous stigma of hypertrichosis as well as disc pathology, genitourinary dysfunction, intraspinal lipoma, etc. are counted (Gregerson 1997).
On the contrary, SBA is a much more severe condition than SBO, and can lead to fatal outcomes. It is linked with various pathologies, such as hypoplasia of the vertebrae, diastematomyelia (split cord malformation), scoliosis, kyphosis and hemivertebrae.
There are three degrees of severity (Aufderheide and Rodríguez-Martín 1998):
- Meningocele: meninges and nerve roots extrude through the neural arch defect, but the spinal cord remains in situ. The lumbosacral region is the most commonly affected site and accounts for 5% of cases of SBA.
- Myelomeningocele: the spinal cord is also extruded. This type constitutes the majority of cases of SBA (about 60%) and affects the L-S segment. It may be associated with hydrocephalus.
- Myelocele: in this case the skin does not close at the level of the vertebral anomaly, hence causing the newborn to succumb shortly after birth as a result of infectious processes. This is the most serious type of SBA and can result in death from infection.
Furthermore, it is worth underlining that for palaeopathologists spina bifida represents a problematic matter because it is difficult to distinguish between its two types: skeletal remains are generically referred to as spina bifida occulta (SBO), since it is not possible to know what external presentation of the anomaly, at the cutaneous level, actually was in life. According to Morse the presence of a meningocele or myelomeningocele causes severe neurological symptoms and is incompatible with a long life, which leads to the conclusion that, whenever an archaeologist finds this defect in an adult skeleton, it is safe to consider the condition as spina bifida occulta (Morse 1978). To this definition Barnes’s can also be added: “The spinal canal is widened with neural tube defect, pushing the edges of the bony cleft outward. In contrast, the spinal canal remains normal, and the edges of the bony cleft are not raised when no neural tube defect is present” (Barnes 1994). The former definition fits SBA, whereas the latter is more adequate for SBO.
From an historical perspective, among the early descriptions of spina bifida feature that by the ancient Greek physician Hippocrates (ca. 460-ca. 375 BC) in the ancient world and by the Dutch clinician Peter van Forest (1522–1597) and the Swiss scholar Caspar Bauhin (1560–1624) in the Early Modern Period (Goodrich 2008; Ashwal 2021). However, its first illustrated description and its very scientific name are to be owed to the work of Nicolaes Tulp (1593–1674) – at a time in which anthropological research did not exist as a separate scientific branch and was still part of the greater family of human anatomy (Papa et al. 2019) –, the famous Dutch anatomist immortalised by Rembrandt’s 1632 painting De anatomische les van Dr Nicolaes Tulp (“The Anatomy Lesson of Dr. Nicolaes Tulp”) exhibited in the Mauritshuis art museum (The Hague, the Netherlands), in his work Observationes Medicae in 1641 (Goodrich 2008). Tulp reported on some cases of spina bifida and used this definition as chapter XXX of this work (Spina dorsi bifida, “Bifid spine of the dorsum”), where he described, with full anatomical arguments, a case of spina bifida aperta (vidimus spinae medullam plane laceram; et nervorum propagines tam varie, per tumorem dispersas, “we saw the spinal medulla completely torn and the nerves’ endings scattered in such varied degrees”, Fig. 6) (Tulp 1641), which resulted in the infant’s death due to what would now be defined an incorrect surgical procedure, namely the ligation and surgical removal of the herniated neural contents.
However, its first complete description is to be attributed to the German pathologist Friedrich Daniel von Recklinghausen (1833–1910), who in 1886 published his work Untersuchungen über die Spina bifida (Goodrich 2008) – without forgetting the contributions to the study of this anomaly by the Sicilian physician
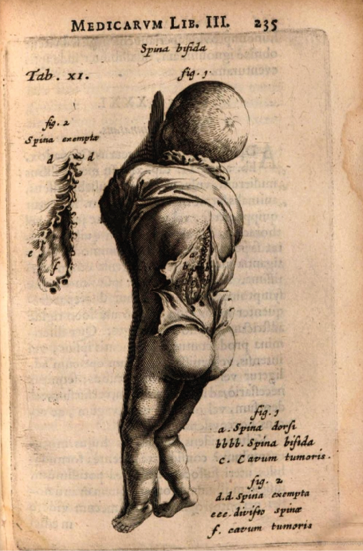
Fig. 6. Illustration of a case of spina bifida aperta from Nicolaes Tulp’s 1641 work, book III, page 235
Giuseppe Muscatello (1866–1951) (Tardieu et al. 2017). Furthermore, Rudolf Virchow (1821–1902), while commenting on the case of a Greek soldier with sacral trichosis (Fig. 7) reported on by Dr Bernhard Ornstein, chief physician of the Greek Army, presented a case he himself had examined, that of a 24-year-old female (Fig. 7): Als ich nunmehr den Rücken präparierte, stellte sich sonderbarerweise heraus, dass unmittelbar unter der behaarten Stelle eine Spina bifida occulta lag, d. h. dass an dieser Stelle die Wirbel an ihrem hinteren Umfange nicht geschlossen waren. An der Stelle der Dornfortsatze der oberen Kreuzbeinwirbel befand sich eine harte Membran; nachdem dieselbe eingeschnitten war, sah ich unmittelbar die Dura mater spinalis vor mir. (“When I now dissected the dorsum, it turned out strangely that immediately below the hairy part there was a spina bifida occulta, i.e. that at this point the vertebrae were not closed at their posterior circumference. In the place of the spinous processes of the upper sacral vertebrae there was a hard membrane; after it had been cut into, I immediately saw the spinal dura mater in front of me” (Ornstein & Virchow 1875).
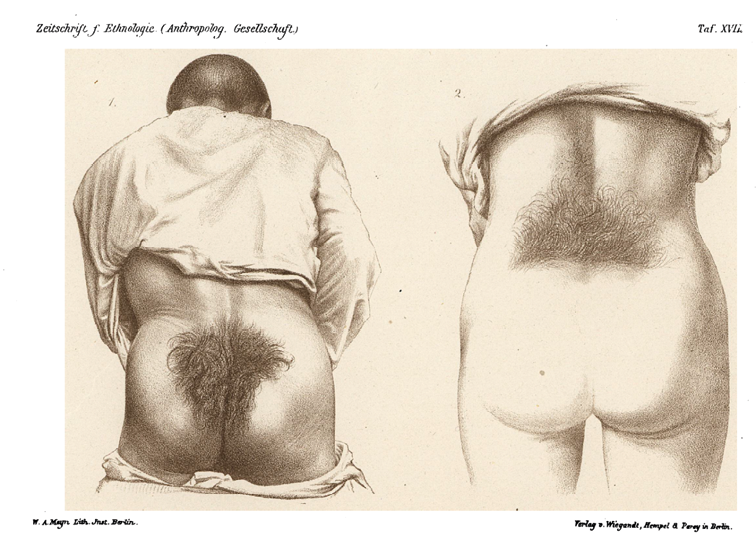
Fig. 7. Illustration of cases of spina bifida occulta in Rudolf Virchow’s work from Zeitschrift für Ethnologie 1875, 7. Bd., Table XXVII, Figs. 1 and 2
With particular reference to SBO, it is described as one of the commonest congenital anomalies affecting the spinal column (Kelty and Henneberg 2022). A recent review indicated a statistically significant increase of this condition after AD 1900 and linked this increase in frequency with relaxed natural selection (Kelty and Henneberg 2022), namely the result of environmental elimination or weakening of specific sources of selection that proved formerly key to the preservation of a particular trait (Staub et al. 2018).
In the case from Leontinoi, while a standard morphological assessment permitted a prima facie diagnosis, unlike in most studies mentioning this anomaly, the implementation of palaeoradiological techniques was stressed. In in-vivo studies on patients in the contemporary clinical setting, MRI and ultrasound imaging are the standard diagnostic techniques, while CT scan imaging has been described as of limited value in the spina bifida in vivo because of its low sensitivy and poor tissue constract, with the further burdern of exposure to iodising radiation for the patients (Trapp et al. 2021). It is generally solely utilised in cases where it proves impossible to sedate a patient or the investigated bone anomaly is severe (Trapp et al. 2021). However, it happens more frequently that following an X-ray or CT scan imaging session for diagnostic purposes, spina bifida can be an incidental report (Manenti et al. 2016). Nonetheless, it should be underlined how CT scan imaging of mummied human remains can actually yield precise information on the presence of spina bifida (Picchi et al. 2022). In the presently studied case, since no patients nor soft tissues were involved, the implementation of X-ray and CT scan imaging helped to better understand the underlying architecture of this congenital anomaly.
Based on these morphological and radiological considerations it can thus be concluded that the described spina bifida sacralis is of the occult type, considering that SBA would be incompatible with the age at death estimated for the individual from Tomb 32.
Additional palaeopathological information on this skeleton’s spine includes the possibility that it may also have been affected by a severe form of scoliosis, formulated at the time of the excavation by observing the in-situ curvature of spine (Palermo 1991), but this notion is to be probably ruled out after an examination of the remnants of the vertebral column and ribs in the laboratory.
As for the exact cause of this vertebral anomaly, it is impossible to identify it retrospectively, since, only having one single line of evidence – in this instance osteological in nature –, and no pathobiographical information on this individual intra vitam nor genetic data, it is preferable to restrain oneself from venturing into the field of aetiology (Galassi and Gelsi 2015).
Excluding causes which are not possible for ancient times (intake of neural tube defect-causing medications such as valproic acid, an antiepileptic) or are less likely (obesity and diabetes, rarer risk factors than they are in the modern world and clearly not showing their non-specific lesions on the discussed skeleton), other aetiologies such as folate deficiency, hyperthermia in the early weeks of pregnancy, or family history of neural tube defects can be carefully considered (Mitchell et al. 2004). As to folate (vitamin B9) deficiency, its role in neural tube defects (NTDs) was unknown until the 1960s when the British paediatrician Richard Worthington Smithells (1924–2002) and obstetric pathologist Elizabeth Hibbard (1928–2019) noted the association (Wald 2011), which ultimately led scientists in the early 1990s to establish that an increased intake of folate or folic acid in the early phases of pregnancy reduces the risk of NTDs (Bentley et al. 2006). As a result, in 1998 the US Food and Drug Administration made it mandatory that folic acid fortified enriched grain products (Bentley et al. 2006), whereas, still in the late 1990s in Sicily, women at risk for recurring neural tube defect were reported in a study not to be aware of the prevention of such outcomes through folic acid supplements (Pepe et al. 1999). While the role of folates in the aetiology of spina bifida was not well-known or understood at the popular level in the Sicilian population, it is important to underline how, on the contrary, the morphological presentation of this neural tube defect was indeed known. The Sicilian physician and ethnologist Giuseppe Pitrè (1841–1916), in his 1896 work Medicina popolare siciliana (“Sicilian Popular Medicine”), reported that spina bifida was called in the Sicilian language “la cusuzza” (standard Italian: “la cosuccia”; English: “the little thing”) and defined it as follows: È un tessuto incancrenito, e se si tocca disattentamente si corre pericolo di far morire il bambino. Si strofina con saliva per tre giorni di seguito; e sparisce al terzo (“It is an encrusted tissue, and if you touch it carelessly you run the risk of killing the child. You rub it with saliva for three days in a row; it disappears on the third day”) (Pitrè 1896). Pitrè’s description seems to refer to the aperta variant of spina bifida in that a protruding mass would account for the word “cusuzza” and the quasi-magical attempts at treating it he described.
Regarding the role of dietary folates in the pathophysiology of this condition, a recent study by Mutlu and colleagues (2020) showed how a Mediterranean Byzantine population which had access to folate-rich food products presented a lower prevalence of spina bifida than other Anatolian populations taken as a comparison.
As for the antiquity of the reported cases, the extensive literature search performed did not yield any reports of this condition in Sicily for the centuries before Christ. This gap in the literature should not lead to an underestimation of the prevalence of this vertebral anomaly in the past as it could be explained by the fact that it may have gone unnoticed by past archaeologists with no to minimal training and/or practical experience in osteoarchaeology, or may simply have not been reported in scientific or multidisciplinary publications due to its being considered unimportant if weighted against other more purely archaeological aspects.
Nonetheless, even though more reports were or will be available in the future, as noted by Henneberg and Henneberg (1999), «[d]espite many published reports on spina bifida occulta, from both historical and modern skeletal collections, it is difficult to compare frequencies of spina bifida occulta across populations and through time», due to the underlined «lack of a clear definition of spina bifida occulta in the sacrum for use in comparative skeletal studies».
Conclusions
This report of a Greek-era Sicilian case of spina bifida sacralis occulta helps to expand knowledge on the presence of this condition in the ancient history of the Sicily. Future reports of this condition might lead to the possibility of an assessment of the prevalence of this anomaly in the midst of the Mediterranean region.
Acknowledgements
The authors wish to express their gratitude to the Leontinoi Archaeological Park (Lentini, Siracusa, Sicily – former director: Lorenzo Guzzardi) and the Superintendence of Syracuse for granting them the possibility of studying the Contrada Pozzanghera burial site. Special thanks go to the Centro Polidiagnostico “San Luigi” (Rosolini, SR, Sicily), in particular to Corrado Protasi and Michela Micieli, for helping with the acquisition of radiological images and their precious assistance.
Conflict of interest
The authors declare no competing interests.
Authors’ contribution
Co-first authors S.M. and E.V. wrote the first draft with E.V. acting as co-supervisor of the thesis of S.M. and having a major role in the methodological planning. E.P., L.G., V.P., D.P. all contributed with archaeological or review remarks, revised the original draft and offered substantial criticism that was incorporated in this manuscript. F.M.G supervised the work, wrote the discussion, contributed to the palaeoradiological analysis together with E.V. and V.P.
Corresponding author*
Francesco M. Galassi, Department of Anthropology, Faculty of Biology and Environmental Protection, University of Łódź, Łódź, Poland, e-mail: francesco.galassi@biol.uni.lodz.pl
 https://orcid.org/0000-0003-2696-293X
https://orcid.org/0000-0003-2696-293X

