Available online at: https://doi.org/10.18778/1898-6773.86.4.02
 https://orcid.org/0000-0001-8987-1838
https://orcid.org/0000-0001-8987-1838
Anthropological Survey of India, 27 Jawaharlal Nehru Road, Kolkata, India
 https://orcid.org/0009-0003-7919-7853
https://orcid.org/0009-0003-7919-7853
Department of Biotechnology, Bodoland University, Kokrajhar, Assam, India
 https://orcid.org/0009-0000-3883-6047
https://orcid.org/0009-0000-3883-6047
PGT, JIPMER (Jawahar Institute of Post Graduate Medical Education and Research), Pondicherry, India
 https://orcid.org/0009-0003-1180-8021
https://orcid.org/0009-0003-1180-8021
Anthropological Survey of India, 27 Jawaharlal Nehru Road, Kolkata, India
 https://orcid.org/0000-0002-2223-9990
https://orcid.org/0000-0002-2223-9990
Anthropological Survey of India, 27 Jawaharlal Nehru Road, Kolkata, India
 https://orcid.org/0000-0001-5373-0400
https://orcid.org/0000-0001-5373-0400
Visiting Professor, Thalassemia & Sickle Cell Society, Hyderabad, India
ABSTRACT: Dyslipidemia is an important risk factor of cardiovascular disease, whereas menopause is a decrease in ovarian follicular activity at the end of reproductive age of the women, which is significantly influenced by hormonal changes brought on by menopause’s impact on serum lipids. This study was undertaken among pre- and post-menopausal Paundra Kshatriya women in Sonarpur, South 24 Parganas, West Bengal, India in order to determine the prevalence of dyslipidemia. 142 adult Paundra Kshatriya women (n pre-menopausal women = 96; n post-menopausal women = 46) were selected from a peri-urban setting of Sonarpur, South 24 Parganas, West Bengal. Anthropometry and arterial pressure data were recorded. Blood samples were collected from study participants who were on 12 hours fasting. 19.79% of pre-menopausal women and 17.39% of post-menopausal women had normal levels of lipids. Prevalence of dyslipidemia was slightly higher (82.7%) among the post-menopausal women compared to pre-menopausal women (80.2%). While high LDL cholesterol emerged as one of the prime causes for dyslipidemia among pre-menopausal women, hypercholesterolemia emerged as one of the prime causes for dyslipidemia among post-menopausal women. Regression analysis revealed a significant impact of 3 factors in pre-menopausal women and impact of 6 factors in post-menopausal women. Though Paundra Kshatriya women maintain a relatively less stressful and high physical activity lifestyle, they exhibited high levels of lipid abnormalities. The peri-urban population is undergoing lifestyle and dietary changes due to a close proximity to the urban centre, Kolkata.
KEY WORDS: Lipid profile, Menopause, Peri-urban population, India.
Cardiovascular disease is a condition of lipid metabolism heavily influenced by dyslipidemia. This can involve either an excess or deficiency of lipoproteins, or both. It is thought to be one of the main risk factors for atherosclerotic disease, particularly coronary heart disease. Low HDL cholesterol and/or high triglycerides are two possible components of dyslipidemia (Dyslipidemia: nhp.gov.in/dyslipidemia_mtl. On the other hand, the absence of menstruation at the end of the reproductive age is known as menopause and is caused by a decrease in ovarian follicular activity. The cardiovascular illnesses linked to menopause are significantly influenced by the hormonal changes brought on by menopause’s impact on serum lipids (Kanwar et al. 2014). Ovarian function is lost after menopause which results in unfavourable changes in vascular endothelial dysfunction, body fat distribution, coagulation, fibrinolysis, as well as glucose and insulin metabolism (Spencer et al. 1977).
Cardiovascular diseases, which are currently the main cause of female mortality, are becoming more common in menopausal women due to contemporary risk factors, such as smoking, obesity, sedentary lifestyles, hypercholesterolemia, and eating habits, as well as an increase in life expectancy (Solimene 2010). After menopause, the lipid profile alterations that take place are linked to an increased risk of cardiovascular disease. Estrogen deficiency is a crucial component of this process. In addition to maintaining a healthy lipid profile, estrogen alters the tone of the blood vessels by producing more nitrous oxide (Taddec et al. 1996). Numerous recent studies show that an increase in cardiovascular risk during menopause is substantially correlated with the evolution of lipid markers. Menopausal women exhibit higher levels of LDL cholesterol, total cholesterol, and apolipoprotein B than premenopausal women do (Bonithon-Kopp et al. 1990; Wu et al. 1990). Menopause may play a role in the adjustment of lipid parameters, as shown by the Framingham study showing that cholesterol levels rose around the time of menopause (Hjortland et al. 1976).
Wang et al. (2016) compared serum lipid levels in pre-menopausal and post-menopausal women and evaluated the relationship between menopause and lipid profiles among the patients in a Beijing hospital. They found that the prevalence rate of dyslipidemia in post-menopausal women was significantly higher compared to pre-menopausal women. The study of Shrestha et al. (2022) in Western Nepal also revealed that prevalence of dyslipidemia was high among post-menopausal women. Various lipids were significantly increased in post-menopausal women compared to pre-menopausal women. A comparative cross-sectional study conducted in Alwar city in Rajasthan, India, revealed a higher prevalence of cardiometabolic risk factors amongst dyslipidemic post-menopausal urban women. Co-existence of dyslipidemia and menopause aggravates the risk condition in post-menopausal women (Parnami and Varma 2021). The risks of atherosclerotic cardiovascular and cerebrovascular diseases in women rapidly increases with age in post-menopausal women. Zhang et al. (2018) found post-menopausal patients were more severely affected compared to pre-menopausal patients in terms of dyslipidemia and systemic inflammation. Jeong and Kim (2022) examined awareness and related factors of dyslipidemia in menopausal women in Korea and found that prevalence of dyslipidemia in menopausal women was high while their awareness was significantly low.
Although there is a substantial number of studies on dyslipidemia in pre- and post-menopausal women there is no, to our knowledge, a single study conducted in a population living in a peri-urban setting in India. This cross-sectional observational study aimed to determine prevalence of dyslipidemia in a pre- and post-menopausal Paudra Kshatriya women in a peri-urban setting of Sonarpur.
Sonarpur is a peri-urban neighbourhood in South 24-Parganas, West Bengal, with excellent bus and rail connections to Kolkata, the State’s capital. The largest group of the study area’s diverse population is the Paundra Kshatriya or Pod (caste). In terms of total socio-economic development, the the Paundra Kshatriya people are regarded as a disadvantaged group. Only a small number of Paundra Kshatriya families are able to support themselves entirely from the income they generate (Singh 2008). The subsistence economy of the Paundra Kshatriya, who live in this area, is heavily dependent upon a variety of occupations. Males primarily work for themselves (33.8%) and in a variety of white-collar jobs (27.33%). Males work in both skilled (17.95%) and non-skilled (13.85%) occupations in significant numbers. Only a small proportion of females work in non-skilled (4.27%), skilled (2.40%), white collar jobs (3.73%), and self-employment (2.93%) occupations. Most women in this group are housewives (86.13%) (Bagchi and Adak 2012).
This cross-sectional observational study was conducted among adult Paundra Kshatriya women. Exclusion criteria were as follows: i) being unrelated to the Paundra Kshatriya (i.e., belonging to other ethnic lineages) and ii) patients with diabetes who take lipid-lowering medication or who have a history of dyslipidemia. Inclusion criteria were the following: i) pre- and post-menopausal unrelated Paundra Kshatriya women and ii) the women who were without regular intake of diabetic and lipid-lowering drug. A standard questionnaire, developed by the authors of this study, was employed, which included questions about eating habits, physical activity, sex, age, and more. Following the presence of one or more abnormal serum lipid readings, dyslipidemia was defined. Cutoff values were used in accordance with NCEP’s (National Cholesterol Education Programme, III, 2001) recommendations, including the following:
1. TG≥150 mg/dl
2. LDL-C≥100 mg/dl
3. HDL-C≤40 mg/dl for men and HDL-C≤50 mg/dl for women
4. TC≥200 mg/dl
This study included 142 adult women aged between 20 and 70 of whom 46 were menopausal and 96 premenopausal. Data on arterial pressure and anthropometry were recorded. Blood samples were taken from unrelated people who had fasted for 12 hours. The samples were examined in the Kolkata laboratory of the Anthropological Survey of India. The Semi-Auto Analyzer, Minitechno, manufactured by Logotech India Pvt. Ltd., was used to perform the analyses.
Anthropometric indices, including body mass index (BMI), waist circumference (WC), and waist-hip ratio (WHR), have been recognized as beneficial screening tools mainly due to an easy access and cost-effectiveness (Kushkestani et al. 2020). We looked at anthropometric measurements such as (a) height (cm), (b) weight (kg), (c) waist circumference (cm), and (d) hip circumference (cm). While taking the measurements, study participants were dressed in light clothing and were not wearing shoes. Martin’s anthropometer rod was used to measure height and a weighing machine equipped with a weighing scale was used to assess weight. The BMI (body mass index) was computed by dividing weight (kg) by height (square metres). A steel tape was used to measure the waist and hip circumference. To determine the relationship between various parameters and dyslipidemia a linear regression was applied. The Venn diagram was created to show how the various dyslipidemia components intersect for pre- and post-menopausal separately. Hypercholesterolemia (serum cholesterol levels of 200 mg/dl) and hyperglyceridemia (serum triglyceride levels of 150 mg/dl) were defined following Joshi et al. (2014). BMI and waist- hip ratios were calculated. T-test and binomial test of equality of proportion were performed to determine whether differences between investigated parameters were statistically significant. The study obtained ethical approval from the Ethics Committee of the Anthropological Survey of India. Once written informed permission had been obtained, all subjects were enrolled.
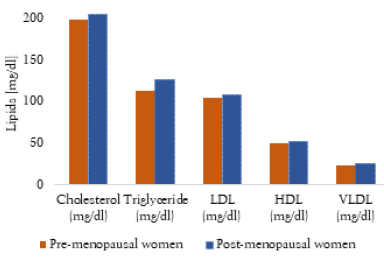
Mean values of various lipids of pre- and post-menopausal women are shown in Table 1 and Figure 1. Post-menopausal women had greater levels of serum cholesterol, serum triglycerides, LDL (low density lipoprotein) cholesterol, HDL (high density lipoprotein) cholesterol, and VLDL (very low density lipoprotein) cholesterol compared to pre-menopausal. However, t-test results showed statistically significant difference between pre- and post-menopausal women in terms of serum cholesterol (t=5.03; p<0.05), serum triglyceride (t=13.88; p<0.05), LDL cholesterol (t=6.88; p<0.05), HDL cholesterol (t=8.78; p<0.05) and VLDL cholesterol (t=11.43; p<0.05).
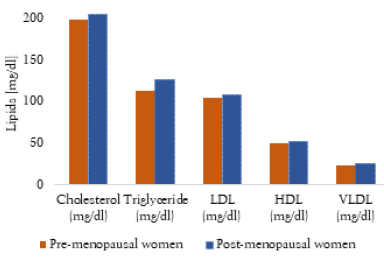
Fig. 1. Mean values of lipids in pre- and post-menopausal women
| Variables | Pre-menopausal (n=96) Mean (SD) |
Post-menopausal (n=46) Mean (SD) |
| Serum cholesterol (mg/dl) | 197.99 (4.64) | 205.59 (9.73) |
| Serum triglyceride (mg/dl) | 112.59 (4.03) | 127.05 (6.49) |
| LDL cholesterol (mg/dl) | 103.62 (2.50) | 108.34 (4.32) |
| HDL cholesterol (mg/dl) | 49.26 (1.50) | 52.33 (2.13) |
| VLDL cholesterol (mg/dl) | 22.50 (0.79) | 24.77 (1.23) |
Table 2 provides general information about study participants based on the presence or absence of dyslipidemia. More than 82 percent of the participants had dyslipidemia. Both pre- and post-menopausal women may attest to this. Additionally, it was discovered that post-menopausal women (82.7%) had a higher prevalence of dyslipidemia compared to pre-menopausal women (80.2%). In the category of subjects with no lipid abnormality, pre-menopausal women showed higher means in the variables like BMI, hip circumference, fasting plasma glucose, serum cholesterol, LDL cholesterol and HDL cholesterol. The rest of the variables showed a reverse trend in this respect. In the category of subjects with any lipid abnormality, post-menopausal women showed higher means almost in all the variables compared to pre-menopausal women excepting in case of BMI and hip circumference. However, t-test results showed statistically significant difference in all the category between women with no lipid abnormality and lipid abnormality among pre-menopausal women, except fasting plasma glucose. Side by side, statistically significant difference is found in most of the category between women with no lipid abnormality and lipid abnormality among post-menopausal women excepting in case of age, hip circumference, serum triglyceride and HDL cholesterol.
| Variables | Pre-menopausal women (n=96) | Post-menopausal women (n=46) | ||
| Study participants with no lipid abnormality (n=19) Mean (SD) |
Study participants with any lipid abnormality (n=77) Mean (SD) |
Study participants with no lipid abnormality (n=8) Mean (SD) |
Study participants with any lipid abnormality (n=38) Mean (SD) |
|
| Age (years) | 34.00 (1.44) | 30.87 (0.60) | 54.25 (2.20) | 52.89 (1.08) |
| BMI | 22.63 (0.85) | 24.63 (0.46) | 22.17 (1.54) | 24.21 (0.68) |
| Waist circumference (cm) | 78.65 (2.15) | 81.42 (1.28) | 79.11 (2.34) | 81.71(1.87) |
| Hip circumference (cm) | 91.91 (1.64) | 94.78 (0.96) | 91.01 (2.63) | 90.17 (1.98) |
| Waist hip ratio | 0.85 (0.01) | 0.86 (0.01) | 0.87 (0.01) | 0.91 (0.02) |
| Systolic blood pressure (mm Hg) | 120.89 (3.73) | 124.73 (2.28) | 148.87 (10.85) | 137.24 (3.04) |
| Diastolic blood pressure (mm Hg) | 77.71 (2.30) | 82.41 (1.49) | 93.87 (4.96) | 87.84 (2.26) |
| Fasting plasma glucose (mg/dl) | 89.81(3.35) | 88.62 (1.86) | 89.63 (2.52) | 92.33 (3.04) |
| Serum cholesterol (mg/dl) | 180.51 (6.76) | 202.31 (5.45) | 176.54 (7.58) | 215.18 (5.64) |
| Serum triglyceride (mg/dl) | 92.75 (7.36) | 117.22 (4.54) | 124.26 (5.43) | 127.66 (7.80) |
| LDL cholesterol (mg/dl) | 88.07 (4.35) | 107.46 (2.77) | 80.07 (7.66) | 113.28 (4.41) |
| HDL cholesterol (mg/dl) | 53.12 (3.52) | 48.30 (1.65) | 51.34 (5.73) | 52.02 (2.34) |
| VLDL cholesterol (mg/dl) | 18.66 (1.24) | 23.45 (0.91) | 22.36 (2.08) | 25.28 (1.42) |
Prevalence of dyslipidemia among the pre- and post-menopausal women is shown in Table 3. While hypercholesterolemia (pre-menopausal: 46.87%; post-menopausal: 69.56%) and hypertriglyceridemia (pre-menopausal: 11.46%; post--menopausal: 21.74%) both were found to be more prevalent among post-menopausal women, high LDL cholesterol (pre-menopausal: 50.00%; post-menopausal: 47.83%) and low HDL cholesterol (pre-menopausal: 24.17%; post-menopausal: 15.22%) occurred in more frequently among pre-menopausal women. However, when dyslipidemia was taken into consideration it was found that prevalence of high LDL cholesterol was highest among pre-menopausal and hypercholesterolemia was highest among post-menopausal women. Binomial test of equality of proportion was calculated between two groups to determine whether there were significant differences between proportions. It was found that difference between the proportions of hypercholesterolemia (0.22±0.09) and hyperglyceridemia (0.11±0.05) was significant, while difference between the proportions of high LDL cholesterol and low HDL cholesterol was not significant.
| Prevalence | Pre-menopausal women (n=96) | Post-menopausal women (n=46) |
| Hypercholesterolemia (mg/dl) | 46.87 | 69.56 |
| Hypertriglyceridemia (mg/dl) | 11.46 | 21.74 |
| High LDL cholesterol (mg/dl) | 50.00 | 47.83 |
| Low HDL cholesterol (mg/dl) | 24.17 | 15.22 |
Venn diagrams were created to illustrate how various dyslipidemia-related factors overlapped in pre- and postmenopausal women (Figures 2a and 2b). Pre-menopausal 4.17% (n=4) and post-menopausal women 8.7% (n=4) showed the presence of three lipid abnormalities (hypercholesterolemia, hypertriglyceridemia and high LDL – cholesterol). About 19.79% (n=19) of pre-menopausal women and 17.39% (n=8) of post-menopausal women had normal levels of lipids. However, 4.17% (n=4) of pre-menopausal women and 6.52% (n=3) of post-menopausal women had all four lipid abnormalities (hypercholesterolemia, hypertriglyceridemia, high LDL-cholesterol, and low HDL-cholesterol).

Fig. 2a. Overlap of individual components according to Venn diagram: pre-menopausal women
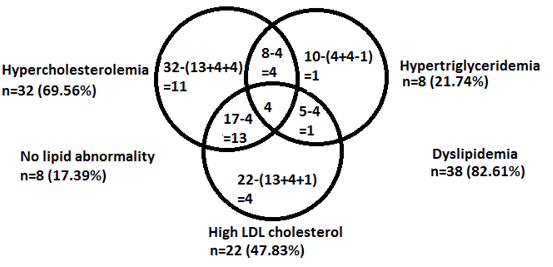
Fig. 2b. Overlap of individual components according to Venn diagram: post-menopausal women
Linear regressions were calculated to examine independent association of factors with lipid abnormalities for pre- and post-menopausal women (Tables 4a and 4b). Among pre-menopausal women BMI was significantly associated with serum cholesterol (SC) and HDL cholesterol. And diastolic blood pressure was significantly associated with LDL cholesterol (Table 4a). Among post-menopausal women waist-hip ratio was significantly associated with serum triglyceride (TG), diastolic blood pressure was significantly associated with LDL cholesterol, fasting plasma glucose was significantly associated with serum cholesterol and HDL cholesterol, and systolic blood pressure was significantly associated with LDL and HDL cholesterol (Table 4b).
| Factors | Serum cholesterol (mg/dl) | Serum triglyceride (mg/dl) | LDL cholesterol (mg/dl) | HDL cholesterol (mg/dl) |
| Age (years) | R2=0.26 | R2=0.27 | R2=0.009 | R2=0.16 |
| F=1.187 | F=1.238 | F=0.632 | F=0.693 | |
| BMI | R2=0.107 | R2=0.002 | R2=0.002 | R2=0.208 |
| F=5.297* | F=0.067 | F=0.071 | F=11.554* | |
| Waist hip ratio | R2=0.096 | R2=0.002 | R2=0.007 | R2=0.003 |
| F=2.098 | F=0.087 | F=0.303 | F=0.112 | |
| Fasting plasma glucose (mg/dl) | R2=0.051 | R2=0.057 | R2=0.005 | R2=0.008 |
| F=2.369 | F=2.648 | F=0.237 | F=0.338 | |
| Systolic blood pressure (mm Hg) | R2=0.032 | R2=0.015 | R2=0.057 | R2=0.015 |
| F=1.441 | F=0.680 | F=2.673 | F=0.679 | |
| Diastolic blood pressure (mm Hg) | R2=0.015 | R2=0.00 | R2=0.080 | R2=0.039 |
| F=0.674 | F=0.011 | F=3.842* | F=1.806 | |
*Results significant at p<0.05 level
| Factors | Serum cholesterol (mg/dl) | Serum triglyceride (mg/dl) | LDL cholesterol (mg/dl) | HDL cholesterol (mg/dl) |
| Age (years) | R2=0.008 | R2=0.002 | R2=0.001 | R2=0.006 |
| F=0.724 | F=0.194 | F=0.083 | F=0.540 | |
| BMI | R2=0.036 | R2=0.009 | R2=0.010 | R2=0.017 |
| F=3.529 | F=0.852 | F=0.903 | F=1.659 | |
| Waist hip ratio | R2=0.002 | R2=0.054 | R2=0.003 | R2=0.014 |
| F=0.210 | F=5.337* | F=0.240 | F=1.318 | |
| Fasting plasma glucose (mg/dl) | R2=0.061 | R2=0.032 | R2=0.022 | R2=0.138 |
| F=6.147* | F=3.087 | F=2.154 | F=15.081* | |
| Systolic blood pressure (mm Hg) | R2=0.004 | R2=0.001 | R2=0.100 | R2=0.042 |
| F= 0.400 | F=0.102 | F=10.500* | F=4.101* | |
| Diastolic blood pressure (mm Hg) | R2=0.027 | R2=0.001 | R2=0.044 | R2=0.016 |
| F=2.578 | F=0.088 | F=4.375* | F=1.532 | |
* Results significant at p<0.05 level
An important modifiable risk factor for cardiovascular disorders is dyslipidaemia. On the other hand, menopause is the permanent cessation of menstruation at the end reproductive life due to loss of ovarian follicular activity. According to Kanwar et al. (2014), menopause-related hormonal changes have a significant impact on serum lipid levels, which are a key factor in most cases of cardiac diseases. A risk factors of coronary heart disease (CHD) include abnormalities of different cholesterol lipoprotein lipids, like high total cholesterol, LDL cholesterol, VLDL cholesterol and triglycerides, and low (LDL) and HDL cholesterol. Raised LDL cholesterol has been found to be a significant predictor of the development of coronary atherosclerosis (Gupta et al. 2017).
Trends in total cholesterol levels were reported by the Global Burden of Metabolic Risk Factors Study between the years of 1980 and 2008. It was projected that throughout this time, total cholesterol levels rose in India as well as in other low- and lower-middle-income nations. Conversely, cholesterol levels decreased in the majority of high-income nations. These trends were discovered through mathematical modelling of sporadic epidemiological research conducted across several nations. The availability of high-quality data from high-income nations (such as the USA, the UK, Germany, Japan, etc.) was facilitated by regular national surveys. In contrast, good-quality epidemiological data are not accessible in low- and lower-middle-income countries, including India; therefore, trends there were determined using probabilistic estimations (cf. Gupta et al. 2017). The results of a study by Pandey et al. (2010) showed that post-menopausal women in Western India had a much greater prevalence of metabolic syndrome compared to pre-menopausal women. Compared to pre-menopausal women, post-menopausal women exhibited significantly higher levels of serum TC, serum TGs, serum LDL, and serum VLDL lipids (Shenoy and Vernekar 2015). Between pre- and post-menopausal women in Kota, Rajasthan, Kanwar et al.’s (2014) study found no discernible change in blood lipid profiles.
The results of our study showed that dyslipidemia affected more than 82 percent of Paundra Kshatriya women, depending on whether it was present or absent. Both pre-menopausal and post-menopausal women may attest to this. In addition, it was found that post-menopausal women (82.7%) exhibited higher rates of dyslipidemia compared to pre-menopausal women (80.2%) although this difference was not statistically significant (x2 = 6.16). The goal of this study was to determine the prevalence of dyslipidemia in pre- and post-menopausal women among the Paundra Kshatriya community of West Bengal’s Sonarpur region, South 24-Parganas district.
Hypertriglyceridemia and hypercholesterolemia were found to be more common in post-menopausal women. In contrast, high LDL cholesterol and low HDL cholesterol were more common in pre-menopausal women compared to post-menopausal women. However, when dyslipidemia was included in the analysis, it was found that pre-menopausal women had the highest frequency of elevated LDL cholesterol while post-menopausal women had the highest prevalence of hypercholesterolemia. The prevalence of dyslipidemia in pre- and post-menopausal Paundra Kshatriya women appears to be on the rise. As a result, the findings of the current study do not support findings reported in other similar studies conducted in India (Pandey et al. 2010; Shenoy and Vernekar 2015; Kanwar et al. 2014).
In many emerging nations, changes in nutrition, demography, epidemiology, and socioeconomic conditions are taking place. Obesity and the metabolic syndrome are becoming more common in adults and children in emerging economy countries as the economic situation improves. According to Mishra and Khurana (2008), urbanization, nutrition change, and decreased physical activity are the key factors. It is interesting to observe that the prevalence of dyslipidemia in the peri-urban population was noticeably high despite adhering to a somewhat less stressful lifestyle exhibiting a high level of physical activity. Given the close proximity of Paundra Kshatriya to Kolkata’s metropolitan core, it is reasonable to suppose that this group is experiencing a change in both eating habits and other aspects of lifestyle.
This study has some limitations. For example, this study was restricted to Paundra Kshatriya which is dominated by peri-urban area. In addition, the sample size was small and, thus, may not be representative of all Paundra Kshatriya population in West Bengal. Moreover, no comparison was made in terms of effects of lipid variation due to food consumption, physical activity, medication and other factors.
This study showed worrying prevalence of dyslipidemia among pre- and post-menopausal Paundra Kshatriya women. Presence of dyslipidemia was slightly higher among the post-menopausal women compared to the pre-menopausal women. Prime cause for dyslipidemia among the pre-menopausal women was high LDL Cholesterol and among the post-menopausal women was hypercholesterolemia. The studied population follow a relatively less stressful and high physical activity lifestyle although it exhibited a very high level of lipid abnormalities. This should be noted that this population is undergoing changes in their lifestyle and dietary pattern due to nearness of urban centre, Kolkata.
Present work got ethical clearance from IHEC (Institutional Human Ethics Committee) of Anthropological Survey of India, Ministry of Culture, Government of India.
Acknowledgements
This paper is an outcome of the project, ”DNA Polymorphism and Diseases (Epidemiological Studies: Cardiac Diseases)” of Anthropological Survey of India (An.S.I.), Kolkata. We gratefully acknowledge the support of the Director of An.S.I. Thanks to all the Paundra Kshatriya subjects who participated in this study. Sincere gratitude to all three anonymous Reviewers for their valuable comments, which substantially helped to improve the presentation of the paper.
Conflict of interest
The authors declare no conflict of interest.
Authors’ contributions
VRR, DKA and NKB conceived the idea of study. NKB, SB and TKB analyzed the data. DKA and NB prepared the Tables and Figure. DKA, NB and TKB took part in drafting the manuscript. VRR, DKA, NKB, NB, SB and TKB all revised and finalized the manuscript.
Funding
Anthropological Survey of India, Ministry of Culture, Government of India
Bagchi NK, Adak DK. 2012. Metabolic Syndrome in a Peri-Urban Population: The Paundra Kshatriya of South 24-Parganas, West Bengal. In: S Biswas, editor. Human Health: A Bio-cultural Synthesis. New Delhi: Concept Publishing Company Pvt. Ltd.159–174.
Bonithon-Kopp C, Scarabin PY, Drane B, Malmejac A, Guize L. 1990. Menopause-related changes in lipoproteins and some other cardiovascular risk factors. Int J Epidemiol 19(1):42–48. https://doi.org/10.1093/ije/19.1.42
Castelli WP. 1988. Cardiovascular disease in women. Am J Obstet Gynecol 158:1553–1560. https://doi.org/10.1016/0002-9378(88)90189-5
Gupta R, Rao RS, Misra A, Sharma SK. 2017. Recent trends in epidemiology of dyslipidemias in India. Indian Heart J 69(3):382–392. https://doi.org/10.1016/j.ihj.2017.02.020
Hjortland MC, McNamara PM, Kannel WB. 1976. Some atherogenic concomitants of menopause: the Framingham study. Am J Epidemiol 103(3):304–311. https://doi.org/10.1093/oxfordjournals.aje.a112228
Jeong J, Kim M. 2022. Awareness and Related Factors of Dyslipidemia in Menopausal Women in Korea. Healthcare 10(1):112. https://doi.org/10.3390/healthcare10010112
Joshi SR, Anjana RM, Deepa M, Pradeepa R, Bhansali A, Dhandania VK, Joshi PP, Unnikrishnan R, Nirmal E, Subashini R, Madhu SV, Rao PV, Das AK, Kaur T, Shukla DK, Mohan V; ICMR-INDIAB Collaborative Study Group. 2014. Prevalence of Dyslipidemia in Urban and Rural India: The ICMR-INDIAB Study. PLoS One 9(5):e96808. https://doi.org/10.1371/journal.pone.0096808
Kanwar G, Kirad S, Chawla L, Jain N. 2014. A comparative study of serum lipid profile between premenopausal and postmenopausal women in Kota, Rajasthan, India. IJRANSS 2(8):61–66.
Kushkestani M, Parvani M, Mosrani SEP, Rezaei S. 2020. The Relationship between Anthropometric Indices and Lipid Profiles in Office Employees. Journal of Sports Science 8:76–82. https://doi.org/10.17265/2332-7839/2020.02.006
Misra A, Khurana L. 2008. Obesity and the Metabolic Syndrome in Developing Countries. The Journal of Clinical Endocrinology and Metabolism 93(1):9–30. https://doi.org/10.1210/jc.2008-1595
Pandey S, Srinivas M, Agashe S, Joshi J, Galvankar P, Prakasam CP, Vaidya R. 2010. Menopause and metabolic sysdrome: A study of 498 urban women from Western India. J Midlife Health 1(2):63–69. https://doi.org/10.4103/0976-7800.76214
Parnami M, Varma K. 2021. Comparative Analysis of Cardiovascular Risk Factors Amongst Pre and Post Menopausal Dyslipidemic Women Residing in Urban Areas. RUHS Journal of Health Sciences 6(4):206–212. https://doi.org/10.37821/ruhsjhs.6.3.2021.396
Shenoy R, Vernekar P. 2015. Fasting Lipid Profile in Pre- and Post-Menopausal women: A Prospective Study. International Journal of Scientific Research 3(9):116–119. https://doi.org/10.17354/ijss/2015/567
Shrestha J, Yadav M, Pokhral BR, Tamang B, Gautam N, Palikhey A, Subedi J, Jha G. 2022. Dyslipidemia in post-menopausal women of Western Nepal: A Community Based Comparative Study. Med S J Med Sci 2(4):26–30.
Singh KS. 2008. People of India. West Bengal, Vol II. Kolkata, Anthropological Survey of India.
Solimene MC. 2010. Coronary heart disease in women: a challenge for the 21st century. Clinics 65(1):99–106. https://doi.org/10.1590/S1807-59322010000100015
Spencer CP, Godsland H, Stevensen JC. 1977. Is there a menopausal metabolic syndrome? Gynecol Endocrinal 11:341–355. https://doi.org/10.3109/09513599709152559
Taddec S, Virdis A, Ghiadonil L, Mattec P, Sudan I, Pernimi G. 1996. Menopause is associated with endothelial dysfunction in women. Hypertension 128:576–582. https://doi.org/10.1161/01.hyp.28.4.576
Wang N, Qin MZ, Cui J. 2016. Lipid profile comparison between pre- and post-menopausal women. Chinese Journal of Cardiology 44(9):799–804. https://doi.org/10.3760/cma.j.issn.0253-3758.2016.09.013
Wu Z, Wu X, Zhang Y. 1990. Relationship of menopausal status and sex hormones to serum lipids and blood pressure. Int J Epidemiol 19(2):297–302. https://doi.org/10.1093/ije/19.2.297
Zhang J, Wang H, Yang S, Wang X. 2018. Comparison of lipid profiles and inflammation in pre- and post-menopausal women with cerebral infarction and the role of atorvastatin in such populations. Lipids in Health and Diseases 17:20. https://doi.org/10.1186/s12944-018-0669-9

