Introduction
Stature is an important anthropometric measurement for several reasons. Body height is a relatively easy anthropological measure to collect. It has been suggested that adult height is a useful marker of variation in cumulative net nutrition, biological deprivation and standard of living between and within human populations (Perkins et al. 2016). Stature is one of the most conspicuous morphological characteristics that has important social, ecological and biological consequences (Little 2020; Raghavan et al. 2022). Height is also a polygenic trait with high heritability (Silventoinen et al. 2003; Jelenkovic et al. 2016; You et al. 2021).
Therefore, anthropologists, actuaries, historians and economists often use height as an indicator of the health status and disease exposure of human populations and it has been shown that greater height is associated with longer lifespan (Finch and Crimmins 2004; Austad 2010). Numerous studies have also demonstrated that stature correlates positively with educational attainment, income, socioeconomic status (SES) and physical health (Peck and Vågerö 1989; Cernerud 1995; Meyer and Selmer 1999; Silventoinen et al. 1999; 2000; Gunnell et al. 2001; Turrell 2002; Heineck 2005; Magnusson et al. 2006; Case and Paxon 2008; Özaltin 2012; Rietveld et al. 2015), although the socioeconomic gradient in adult height has declined in affluent countries (Ayuda and Puche-Gil 2014; Öberg 2014; Perkins et al. 2016).
It has been established that adult height and cardiovascular disease (CVD) mortality are inversely correlated (Paajanen et al. 2010). Shorter individuals are also more vulnerable to type 2 diabetes (Lawlor et al. 2002; 2004). Nonetheless, it should be noted that not all authors agree that shorter people are more prone to CVD as individuals of similar body proportions and body mass index (BMI) should be compared with each other (Samaras 2013). Interestingly, the extent to which tallness is associated with health indices and survival remains unclear since recent studies have challenged this assumption (Miller et al. 2002; Rollo 2002; Samaras et al. 2003; Bartke 2012; 2017; Salaris et al. 2012). However, many studies have reported that taller people are healthier and live longer compared to their shorter counterparts (Davey Smith et al. 2000; Gunnell et al. 2001; Finch and Crimmins 2004; Kemkes-Grottenthaler 2005; Özaltin 2012; Perkins et al. 2016; Marco-Gracia and Puche 2021). This view is popular among anthropologists and physicians. Nevertheless, studies on the relationship between adult stature and longevity have yielded conflicting findings.
The present study aims to determine the association between self-reported height and lifespan in the Polish population. Our research has the potential to contribute to the anthropological literature by using a large and representative dataset and by employing better statistical methods.
Materials and methods
Data on 848,860 individuals, including 483,512 men (57%) and 365,348 women (43%) were collected. The data were obtained from two electronic databases at the Ministry of Internal Affairs and Administration in Warsaw: (1) the Universal Electronic System for Registration of the Population (sex, date of birth and death) and (2) signalments in the census obtained from identity card offices throughout Poland (adult height in cm declared on the identity card of a deceased person).
Extreme values of height (<140 cm for men; <130 cm for women) were excluded from the analysis. After excluding a small proportion (<0.06%) of records due to missing data or obvious errors, we examined records for 848,387 individuals (483,281 men, age range: 20-110 years, born between 1897 and 1984; 365,106 women; age range: 20–112 years, born between 1896 and 1984). All of these records include data on adult deaths in the years 2004–2008 in Poland.
Lifespan (in years) was calculated as the difference between the date of death and the date of birth. After the elimination of the cohort effect, the sample was divided into five height classes using centiles: very short (0–20), short (21–40), medium (41–60), tall (61–80) and very tall (81–100). Height was standardized on year of birth to sex-specific Z-scores in order to eliminate the effects of secular trends in stature. Subsequently, standardized residual variance was used. Pearson’s r coefficients of correlation were calculated. The differences between sexes and among five height classes in lifespan were evaluated with two-way ANOVA and post hoc Tukey’s test. The effect size was estimated using partial eta squared (η2).
The collected data have several important advantages. First, the study sample is very large and representative for the entire population. Second, the research material includes typical causes of death as all records were analyzed, regardless of the cause of death. It should be emphasized that the use of declared stature instead of measured height is acceptable. Although it is true that males often overestimate their height (Cizmecioglu et al. 2005), these effects are especially pronounced in dating services or in studies on physical attractiveness. In general, women only marginally over- or underestimate their height (Brunner Huber 2007). Moreover, it has been shown that data on self-reported height tend to be more reliable when stated for legal and official purposes, and especially in such large samples (Krzyżanowska and Umławska 2002; Bowring et al. 2012; Olfert et al. 2018). Third, in this study data on the exact dates of birth and death were certified by relevant documents. Therefore, the collected data are reliable and the information concerning lifespan is credible.
Results
Body height and lifespan were normally distributed. Men were taller than women (171.6 ± 6.6 cm versus 159.6 ± 6.2 cm; F = 1.14; p < 0.001) and had shorter lives (67.9 ± 13.8 years versus 75.0 ± 12.7 years; F = 1.19; p < 0.001).
Before the elimination of the effects of secular trends in body height, an inverse correlation was found between the declared height and lifespan (Pearson’s r = –0.304, p < 0.001 for men; r = –0.258, p < 0.001 for women). The values of lifespan and declared height before the elimination of the cohort effect are shown in Table 1.
Sex was the most important factor affecting lifespan, whereas body height and the interaction between height and sex had relatively small effects on lifespan. The effects of height on lifespan were 16.5 times weaker than the effects of sex (Table 2). After allowing for the cohort effect, medium men exhibited the longest lives among men, whereas very short women had the longest lives among women (Fig. 1).
| Lifespan | Men | Women | ||||
| N | Mean | SD | N | Mean | SD | |
| <50 | 55603 | 175.7 | (6.8) | 16405 | 163.3 | (6.1) |
| 50-54 | 37551 | 173.7 | (6.3) | 14485 | 161.8 | (5.7) |
| 55-59 | 47715 | 172.9 | (6.2) | 21737 | 161.6 | (5.6) |
| 60-64 | 44072 | 172.1 | (6.1) | 21799 | 161.3 | (5.6) |
| 65-69 | 55889 | 171.2 | (6.0) | 30165 | 160.6 | (5.6) |
| 70-74 | 71313 | 170.8 | (6.0) | 46338 | 160.1 | (5.7) |
| 75-79 | 75537 | 170.3 | (6.1) | 66739 | 159.5 | (5.9) |
| 80-84 | 56442 | 169.7 | (6.4) | 72112 | 158.8 | (6.0) |
| 85-89 | 26644 | 169.3 | (6.7) | 45436 | 158.1 | (6.2) |
| 90-94 | 9649 | 168.2 | (6.9) | 21448 | 156.8 | (6.3) |
| 95-99 | 2510 | 167.3 | (7.0) | 7269 | 156.2 | (6.3) |
| >100 | 373 | 166.7 | (6.8) | 1177 | 155.3 | (6.5) |
| Height class | Men | Women | ||
| N | Mean (SD) | N | Mean (SD) | |
| Very short | 96655 | 68.05 (13.96) | 73021 | 75.91 (13.42) |
| Short | 96657 | 66.58 (13.98) | 73021 | 73.89 (13.09) |
| Medium | 96656 | 68.87 (14.29) | 73021 | 75.00 (12.10) |
| Tall | 96654 | 66.39 (13.45) | 73022 | 74.05 (13.22) |
| Very tall | 96659 | 68.24 (15.15) | 73021 | 75.83 (12.31) |
| Two-way ANOVA | ||||
| F | p | partial η2 | ||
| Sex | 59620.0 | <0.0001 | 0.066 | |
| Height | 812.0 | <0.0001 | 0.004 | |
| Interaction | 106.0 | <0.0001 | 0.001 | |
All of the vertical (e.g. very short men versus short men and so on) and horizontal (e.g. very short men versus very short women and so on) differences between pairs of means were statistically significant (the post hoc Tukey’s test, p < 0.001 for all compared pairs of means).
After the elimination of the cohort effect, no correlation between height and lifespan (Pearson’s r = –0.0012, p > 0.05 for men; r = –0.0004, p > 0.05 for women; Fig. 2A and 2B, respectively) was found.
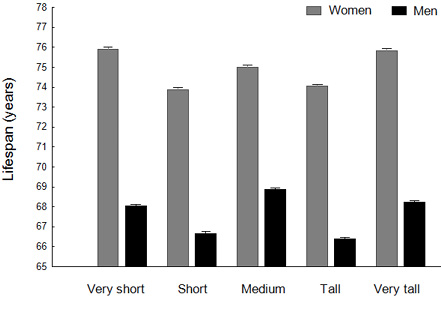
Fig. 1. Differences between sexes and among five height groups in lifespan after the elimination of the cohort effect. Means ± 95% CI are shown. Differences between all pairs of means were significant (post-hoc Tukey’s test, p < 0.001)
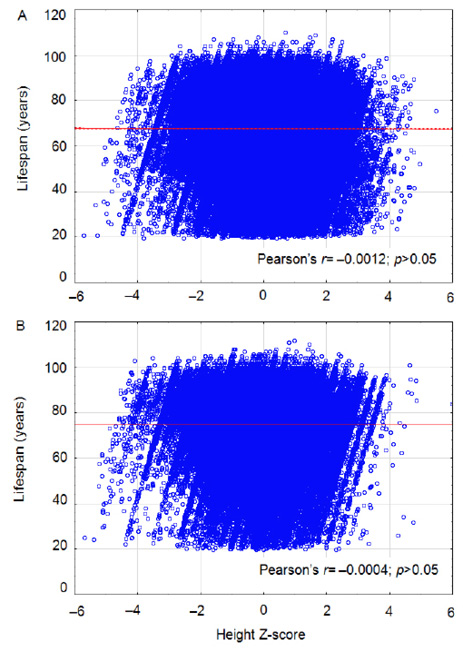
Fig. 2. No correlation between standardized height (Z-scores) and lifespan in men (A) and women (B)
Discussion
A multitude of studies have investigated the relationship between stature and later outcomes in life, including survival. Interestingly, this research has revealed that taller individuals do not have a longevity advantage over their shorter counterparts, which is in line with several studies (Wilhelmsen et al. 2011; Salaris et al. 2012; He et al. 2014).
In our previous articles (Chmielewski 2016; Chmielewski and Borysławski 2016; Chmielewski 2022; 2023), we did not address the problem of the variance of year of birth on stature and we did not express the values of height as standardized residual variance derived from linear regression. Therefore, the current study contributes to previous research by eliminating the cohort effect and, thus, evaluates the association between adult height and lifespan more appropriately.
No correlation between self-reported height and lifespan was found in this study. One possible explanation is that the costs of taller stature cancelled out the well-known benefits, while the benefits of shorter height were too modest to matter (Table 3). Considering that the level of cancer diagnosis and treatment is highly unsatisfactory in Poland, taller individuals are at a disadvantage. Thus, greater height is not associated with longer lifespan in the studied population.
| Benefits of taller height | Benefits of shorter height |
| Taller stature reflects biological quality and is associated with better childhood nutrition and higher SES, including income, remuneration and educational attainment | Fewer cells in the body; the total number of somatic cells predicts the relationship between adult height and cancer risk (Nunney 2018) |
| Lower maximum oxygen uptake, lower heart rate and lower basal metabolic rate | Reduced GH/insulin/IGF-1 signaling and less active mTOR (van Heemst et al. 2005; Bartke 2012) |
| Taller individuals are less vulnerable to atherosclerosis and cardiovascular disease (Paajanen et al. 2010) | Shorter nonagenarians have longer telomeres (Maier et al. 2005), and shorter telomeres are a risk factor of cancer |
| Taller individuals are stronger, run faster,have better jumping ability, are better swimmers and fighters. In our evolutionary past, they provided better security and more resources (e.g. food, water, goods) for their sexual partners and offspring | Shorter people have faster reaction times, greater stability, lower risk of falls, greater endurance and reduced back problems. They are better endurance runners. Furthermore, hip fractures are more common in taller individuals |
It has been established that many factors and processes contribute to human height, including genetic, epigenetic, nutritional, ecological and social factors such as pathogens, parasites, stress level, amount of sleep, diseases or disorders. It should be noted that not only environmental and lifestyle-related factors, such as an unhealthy diet and malnutrition, but also genetic disorders (e.g. Down syndrome, Russel-Silver syndrome, Noonan syndrome, Turner syndrome, Prader-Willi syndrome and dwarfism) and physiological dysfunctions, such as growth hormone (GH) deficiencies, usually result in short stature.
Beard and Blaser (2002) contended that infectious diseases in childhood can negatively affect adult stature. For instance, a number of studies have shown that adults who suffered from diarrhea and dehydration during childhood were significantly shorter than those who did not have these problems. Also a study by Martorell and associates (1975) demonstrated that in Guatemala children relatively free from diarrhea during the first seven years of life were roughly 4 cm taller compared to those children who often suffered from diarrhea. Interestingly, it has been estimated that each episode of diarrhea in childhood is associated with a decrease in adult height by approximately 0.6 cm (Black et al. 1984). Moreover, several other studies have reported that infectious diseases in the first years of life are important factors affecting stature. Clinical observations suggest that certain medical problems and conditions, such as chronic granulomatous disease (CGD), can also result in diminished final height.
Epidemiological and clinical studies have provided evidence that taller stature is linked to an increased risk of cancer as well as decreased survival (Kabat et al. 2013; Wirén et al. 2014; Sohn 2016) even though it is unclear why taller people are more likely to develop cancer and die. However, a number of tentative explanations can be offered. For example, taller and larger individuals have consistently more somatic cells compared to their shorter and slimmer counterparts. Indeed, it has been established that the total number of cells in the body can predict the relation between body size and cancer (Nunney 2018). This is because a higher number of cells in the body increases the risk factor for DNA damage and somatic mutations.
Furthermore, an organism that accumulates extra senescent cells, e.g. a tall and overweight person who is getting older, is more likely to reach higher levels of chronic systemic inflammation (CSI), which can be detrimental to health. CSI and senescence-associated secretory phenotype (SASP) play an important role in aging, promote cancer and increase the risk of other age-related pathologies such as CVD and neurodegenerative disorders (Chmielewski 2018; Chmielewski and Strzelec 2018). Normal growth and development depend on GH/insulin/IGF-1 signaling and mammalian/mechanistic target of rapamycin (mTOR). However, these signaling pathways, when up-regulated, can stimulate cancer development and progression (van Heemst et al. 2005; Bartke 2012; 2017; Tian et al. 2019; Zou et al. 2020).
Growth is physiologically costly and among mammals smaller individuals (within the same species) tend to have lower mortality rates (Rollo 2002). For example, dogs and mice have been studied for years and smaller ones live longer (Miller et al. 2002; Bartke 2012). Interestingly, several studies have reported that primates on CR exhibit reduced body fat and increased insulin sensitivity. CR also reduces bone mass, muscle mass, muscle size and strength (Villareal et al. 2006; Weiss et al. 2007; Kemnitz 2011; Austad 2012). Simultaneously, CR extends lifespan (Anderson et al. 2009; Colman et al. 2009; Mattison et al. 2017), even though not all authors agree.
A number of studies have also suggested that taller people are less likely to reach advanced ages (Samaras et al. 2003; Wilhelmsen et al. 2011; Salaris et al. 2012; He et al. 2014). It is possible that the correlation between taller height and lower mortality is incidental to increased life expectancy. Nowadays people tend to live longer due to better sanitation, education, hygiene, nutrition and advances in preventive and therapeutic medicine (Kirkwood 2017). Taller individuals may benefit more from these advances as they score better in terms of SES.
According to Samaras, who studied various human populations and ethnic groups, short individuals tend to live longer (Samaras et al. 2003; Samaras 2013), especially if they are slim and maintain a healthy lifestyle. Similarly, Salaris and colleagues (2012) reported that shorter men lived about 2 years longer than their taller counterparts. Similarly, Holzenberger and associates (1991) found that shorter Spanish men lived longer than taller ones. These authors tracked the mortality of 1.3 million men over a 70-year period. However, Austad (2010) argues that Samaras reached his conclusion by comparing heights of different groups of people (e.g. different sexes or ethnic groups) within a given country. Due to variation in hormonal milieu, diet, lifestyle and multiple other factors, it is difficult to evaluate the claim that smaller people live longer in the face of a mountain of opposing epidemiological evidence. However, one can argue that this mountain of opposing data is based on mortality studies that did not track the entire cohorts to advanced ages or until death.
He and associates (2014) investigated a population of over 8,000 Japanese Hawaiian elderly males. Based on a 40 year follow up study, they found that shorter men had lower mortality rates and lived longer. Likewise, Wilhelmsen and collaborators (2011) tracked a group of 67-year old Swedish men to 90 years of age. They concluded that individuals who were shorter at baseline were more likely to reach age 90 compared to taller men. Gavrilova and Gavrilov (2008) probably summarized the situation accurately when they pointed out that: “Historical demographers are confident that small body size is associated with increased mortality, while biologists are firmly convinced that a small body size is preferable for longevity”. These researchers found that the highest percentage of centenarians were average in height, which is in agreement with the current study in the case of men. These results also suggest that tall people are less likely to reach advanced ages.
The present study has several limitations that should be noted. First, only self-reported height was used, even though adults often overestimate their stature. Second, older people can also overestimate their stature. Adults lose about 1 cm every 10 years after age 40, and height loss is even more rapid in later stages of ontogeny (Chmielewski et al. 2015a; 2015b; 2016). Since a lot of people do not measure themselves regularly, it is possible that many of them provided outdated information. If so, the actual height was shorter than the self-reported height and the hypothesis that taller people live longer was favored. Third, the collected data vary with respect to the age at which height was declared as this information was unavailable in the current study. We assume that adult height declared on the identity card corresponds with the actual values. Finally, this analysis did not consider potentially significant confounding factors, such as BMI, lifestyle, the cause of death and SES, because these data were not available. Given that shorter individuals score worse in terms of SES, it is rather intriguing that in our study we did not find that taller individuals live longer than their shorter counterparts. Future studies may expand on this research by addressing the limitations of this study.
Conclusions
No correlation between body height and lifespan was found. The effects of sex on lifespan were nearly 17 times stronger than the effects of height, indicating that greater height was not associated with longer lifespan in the studied population. Thus, these results do not support the hypothesis that taller individuals have a longevity advantage.
Conflict of interest
The authors declare that they have no conflict of interests.
Authors’ contributions
PPC conceptualized and designed the study, collected the data, interpreted the results, wrote the manuscript and revised it for important intellectual content. KB conceived the study, supervised the research and reviewed the manuscript. SK performed the statistical analyses, interpreted the results and critically reviewed the manuscript.
 https://orcid.org/0000-0002-6995-123X
https://orcid.org/0000-0002-6995-123X

